Eur Heart J:低卒中风险心房颤动患者口服抗凝剂的疗效
2022-03-11 MedSci原创 MedSci原创
在卒中风险较低的患者中,与不治疗或接受VKA治疗相比,NOAC治疗可能带来积极的净临床获益,这一问题可以通过随机对照试验进行检验。
心房颤动(AF)患者卒中的风险增加五倍。然而,患者之间的风险差异很大,可以使用CHA2DS2-VASc评分进行估计。CHA2DS2-VASc评分基于六个赋值为1分的特征:年龄(65-74)、女性、充血性心力衰竭、高血压、血管疾病和糖尿病,以及两个赋值为2分的特征:年龄≥75岁和既往的卒中/短暂性脑缺血发作(TIA)/栓塞。如果该评分以及卒中风险超过一定水平,则认为口服抗凝剂(OAC)治疗在卒中预防方面的益处超过与治疗相关的出血风险。目前对于卒中风险较低的心房颤动(AF)患者(一个与性别无关的CHA2DS2-VASc分数)是否应接受口服抗凝剂治疗尚无共识。

近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,研究人员在瑞典、丹麦、挪威和苏格兰进行了一项多国队列研究。
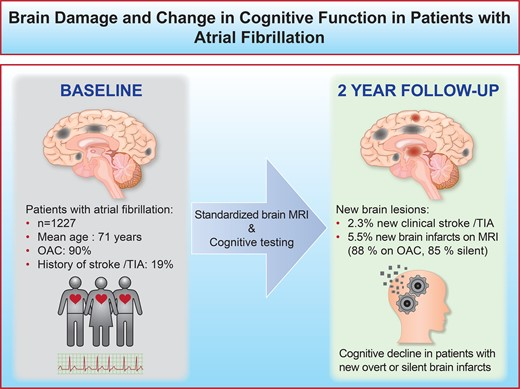
该研究总共纳入了59 076名被诊断为低卒中风险的AF患者。研究人员使用逆概率加权(IPTW)Cox回归评估使用非维生素K拮抗剂口服抗凝剂(NOAC)、维生素K拮抗剂(VKA)治疗或不治疗期间卒中或大出血的发生率。

在未经治疗的患者中,缺血性卒中发生率为0.70人/100人每年,出血发生率为0.70人/100人每年。与未接受NOAC治疗相比,NOAC治疗后的卒中发生率较低[风险比(HR)为0.72;95%置信区间(CI)为0.56-0.94],颅内出血(ICH)发生率未增加(HR为0.84;95%CI为0.54-1.30)。与未接受VKA治疗相比,VKA治疗的卒中发生率往往较低(HR为0.81;95%CI为0.59-1.09),而ICH的发生率在VKA治疗期间较高(HR为1.37;95%CI为0.88-2.14)。将NOAC与VKA治疗比较,卒中发生率相似(HR为0.92;95%CI为0.70-1.22),但NOAC治疗期间ICH发生率较低(HR为0.63;95%CI为0.42-0.94)。
这些观察性数据表明,在卒中风险较低的患者中,与不治疗或接受VKA治疗相比,NOAC治疗可能带来积极的净临床获益,这一问题可以通过随机对照试验进行检验。
原始出处:
Joris J. Komen,et al.Oral anticoagulants in patients with atrial fibrillation at low stroke risk: a multicentre observational study.European Heart Journal.2022.https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehac111/6546013
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#卒中风险#
40
#口服抗凝剂#
48
#ART#
35
#HEART#
37
#心房#
56