PLoS One:主动式经皮骨传导装置的患者报告的长期益处
2020-11-22 AlexYang MedSci原创
最近,有研究人员评估了使用主动经皮骨导装置康复患者的与听力相关的生活质量、患者满意度和佩戴时间的长期益处,并将不良事件和听力学结果作为次要结果报告。
最近,有研究人员评估了使用主动经皮骨导装置康复患者的与听力相关的生活质量、患者满意度和佩戴时间的长期益处,并将不良事件和听力学结果作为次要结果报告。
研究为回顾性、单项研究,包括了16名有传导性或混合性听力损失的成人,装置使用时间均值为51.25个月。研究结果表明,与听力相关的生活质量在SSQ12-B的所有子量表中都得到了显著改善,总体平均得分为2.95分。用APSQ测量的患者满意度平均为8.8分。另外,佩戴时间在个体间差异很大;即与受过高等教育的患者相比,教育水平较低的患者似乎使用设备的时间更长。研究人员记录了8个轻微的不良事件,并在随访期间全部解决。在最后一次随访中,65dB下测量的单词识别得分的平均增益为75.9%,而语音接收阈值降低了35.1dB。
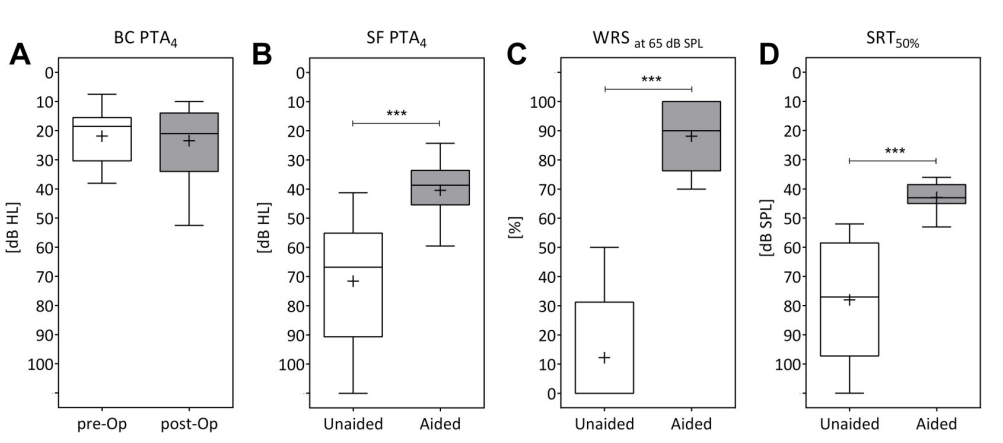
最后,研究人员指出,即使在数年后,患者报告中在与听力相关的生活质量和设备满意度方面均有显著的益处。结合轻微不良事件的低发生率和显著改善的听觉结果,研究人员认为该装置是听力康复中一个舒适和有效的选择。
原始出处:
Julia Hundertpfund, Jens Eduard Meyer , Attila Óvári et al. Patient-reported long-term benefit with an active transcutaneous bone-conduction device. PLoS One. Nov 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Plos one#
57
好文章
77
嗯嗯,好!
0
实用
90