脑中风又叫脑卒中,是一种突然起病的脑血液循环障碍性疾病,也叫脑血管意外。是由各种诱发因素引起脑内动脉狭窄,闭塞或者破裂,而导致急性脑血液循环障碍,又可把脑卒中分为出血性(脑出血和蛛网膜下腔出血)脑卒中以及缺血性脑卒中(脑血栓和脑脑梗塞)。

中风需要康复。中风后康复是一个多学科方法的共同作用过程,旨在帮助恢复日常生活活动(ADL),并改善社会互动,运动疗法是康复的重要组成部分。运动疗法的重点通常是手臂功能和步态的恢复。坐姿平衡是ADL恢复的一个重要预测因子。即使在中风后的慢性期,坐姿平衡也会持续受损,躯干功能也会受损。此外,研究表明,通过强化治疗,如更多的治疗时间和更多的重复次数,ADL可以得到改善。改善坐姿平衡和躯干功能是中风后康复的重要组成部分。研究表明,运动学习原则的结构化实施将有助于改善坐姿平衡和躯干功能。本文开发了一种新的康复技术治疗概念,在一种新开发的称为T型椅的设备上提供坐姿平衡疗法。它允许在没有软件或电子硬件的情况下进行非自动化的移动,T-Chair提供反馈,并提供不同的重复次数,从而实现针对患者的强化治疗。
本文研究了使用T型椅进行技术支持的坐姿平衡疗法的可行性、安全性和潜在有效性。对中风后慢性期的参与者进行了一项单中心试点随机对照试验(RCT),主要目的是调查T型座椅增强坐姿平衡疗法的可行性和安全性。第二个目标是评估与仅常规护理相比,技术辅助治疗是否能改善中风后参与者的坐姿平衡、躯干功能、活动能力、功能平衡、力量和日常生活能力。本文发表在《Journal of NeuroEngineering and Rehabilitation》
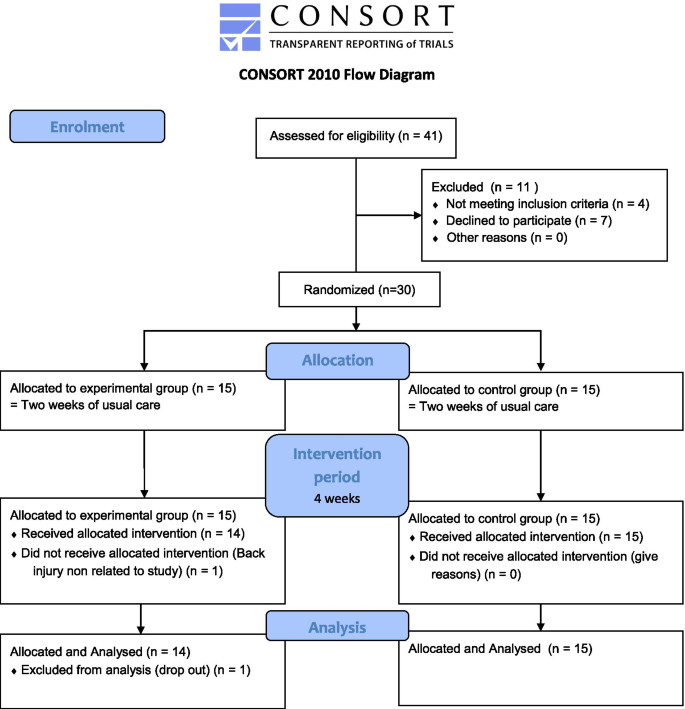
参与者于2020年7月至11月招募。在康复中心和研究地点附近的理疗机构分发了带有研究信息和联系方式的传单和海报。 一名研究人员联系了潜在的候选人,以进一步解释这项研究。确认合格后,从研究志愿者处获得书面知情同意书。这项研究是在比利时康复中心的一个专用房间内进行的,该中心提供门诊治疗。目标是招募30名中风后慢性期的参与者。将参与者随机分配到两个不同的组,实验组和对照组。
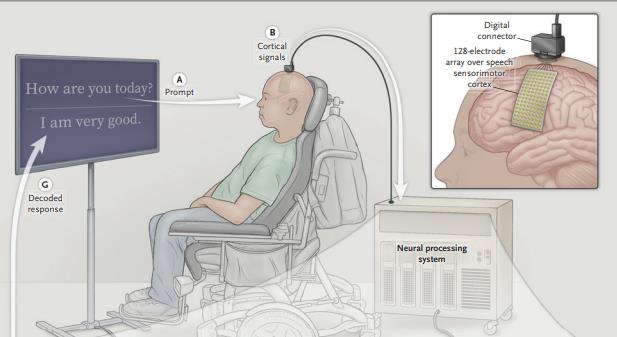
实验组的治疗采用了一种新的康复技术原型,称为T型椅。T-Chair是一种提供视觉反馈的仪器化机器人座椅。阀座提供稳定或不稳定的表面,并允许阀座表面在前后和横向方向上移动。座椅倾斜机构由两对圆形轨道组成,安装在上方并相互垂直,以允许相对运动。第一对圆形轨道安装在矢状面上,而第二对安装在前平面上。该系统允许座椅围绕前轴和矢状轴倾斜(或球形移动)。结构不允许座椅绕垂直轴旋转。从起始位置开始的前后和横向最大可能倾斜为10°。在座椅中,64个传感器(美国Tekscan的FlexiForce A401力传感器)通过检测压力中心的运动,永久性地测量患者坐着时的运动。在治疗过程中,T型椅在向前、向后和侧向运动中提供压力中心运动范围的视觉反馈。T型座椅包括专门设计的游戏,以刺激和激活参与者。游戏的目标是根据屏幕上显示的目标,在重心转移时保持平衡并改善压力中心的运动范围。T型椅的有两个外壳:一个柔性织物盖;一个稳定的硬塑料盖,保护电子设备和电机单元。电机单元由电机单元组成,电机单元由两个混合式步进电机单元组成,驱动T型座椅的主动运动,并配有安全和传感器模块,以保持对运动的安全和明确控制。
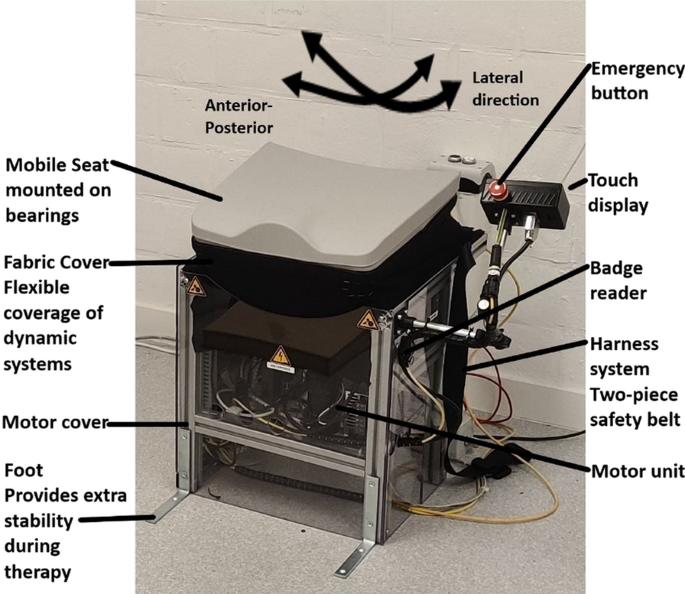
T型椅系统
收集基线数据,如年龄、中风类型和部位、共病、优势手、教育水平和性别。参与者接受了认知(蒙特利尔认知评估)和抑郁水平(患者健康问卷)的筛查。在三个时间点对所有参与者进行测试,干预前两次(称为基线和干预前),间隔两周,干预后一次,干预开始后四周。两项干预前测试旨在确定参与者在本研究中使用的结果是否稳定。四周后实验组结果的变化可归因于研究干预。所有结果均采用临床测量工具或问卷进行评估。治疗师根据六分Likert量表(从差到优)对参与情况进行判断。依从性采用临床医生依从性评定量表进行评估。
研究流程
治疗师为确保参与者安全而采取的所有干预措施均在每次治疗后进行记录。治疗师使用视觉模拟疲劳量表评估疲劳,范围从0到10,其中0表示无疲劳,10表示最严重的疲劳。调查了一般性疲劳,特别是腿部和躯干疲劳。Borg自感劳累评分评估劳累,其评分范围为6到20。6分表示不劳累,20分表示最大劳累。由于坐姿平衡和躯干训练是T型椅治疗的核心组成部分,临床数据的主要结果测量是坐姿平衡和躯干功能。我们使用躯干损伤量表(TIS)对坐姿平衡和躯干功能进行了调查 。步态在三个不同的方面进行评估:步态能力、速度和耐力。使用改良的Ashworth量表评估不同肌肉群的张力,包括肘屈肌和伸肌、髋屈肌和内收肌、膝屈肌和伸肌以及踝跖屈肌。
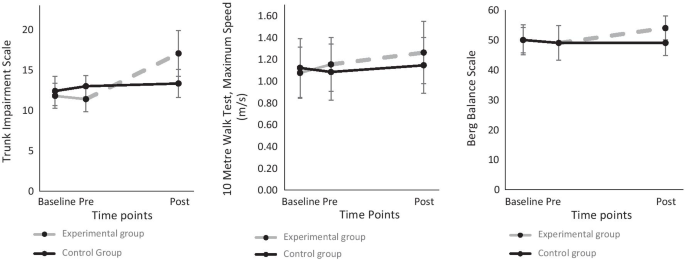
TIS总分随时间变化;最大步速随时间的演变;功能平衡随时间的变化
总共招募了30名参与者,29人完成了试验(实验组:n = 14; 对照组:n = 15). 在基线检查时,各组之间没有差异。参与者和治疗师对治疗进行了可行性评估。坐姿平衡治疗期间未发生严重不良事件。干预前后的临床结果变化表明,实验组在坐姿平衡和躯干功能方面比对照组有所提高,躯干损伤量表(平均分(SD)为7.07(1.69);P < 0.000); 通过10米步行测试评估的最大步态速度(平均步态速度0.16m/s)。
研究结果表明,用躯干损伤量表(TIS)测量,T型座椅对躯干功能有积极影响。改善躯干功能和坐姿平衡是T型座椅的主要重点。实验组的TIS平均改善7分,最高23分(31%),而对照组的平均改善仅为0.33分(1.4%)。这种有利于实验组的改善与临床相关。对于TIS,中风后慢性期的临床意义差异为3.5分。对照组中只有一名参与者相比,所有14名实验参与者都超过了该阈值。专为训练坐姿平衡和躯干功能而设计的T型座椅实现了其目标。
研究表明,技术支持的坐姿平衡疗法是可行和安全的,并且在中风后慢性期提供常规护理的同时,改善社区中风幸存者的躯干功能、步态和功能平衡。通过增加专门针对中风后患者的游戏种类,可以改善游戏应用。为了改善反馈,可以生成标准化报告,并通过电子邮件或集成应用程序发送给患者。应实施进一步的可取改进,例如允许单手使用,使培训更具挑战性,减少技术障碍,并提供独立培训所需的资源。没有严重不良事件或其他安全问题。T-Chair的目的是实现强化的独立培训,在纳入我们研究中得出的反馈后,将更有可能实现这一点。在这项研究中,两组的Barthel指数中位数均高于18分,相当于ADL的高功能水平。因此,这组中风后晚期患者能够非常享受这项技术支持的坐姿平衡疗法。
总之,技术支持的慢性中风患者坐姿平衡训练是可行和安全的。在常规护理的基础上,进行为期四周、12个疗程的计划,对躯干功能、最大步速和功能平衡都有好处。
Thijs, L., Voets, E., Wiskerke, E. et al. Technology-supported sitting balance therapy versus usual care in the chronic stage after stroke: a pilot randomized controlled trial. J NeuroEngineering Rehabil 18, 120 (2021). https://doi.org/10.1186/s12984-021-00910-7
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#常规护理#
53
#对照试验#
50
#对照#
58
#随机对照试验#
38
高质量研究,读起来真爽,谢谢梅斯
60
中风是俗称,应该称为缺血性卒中吧
55