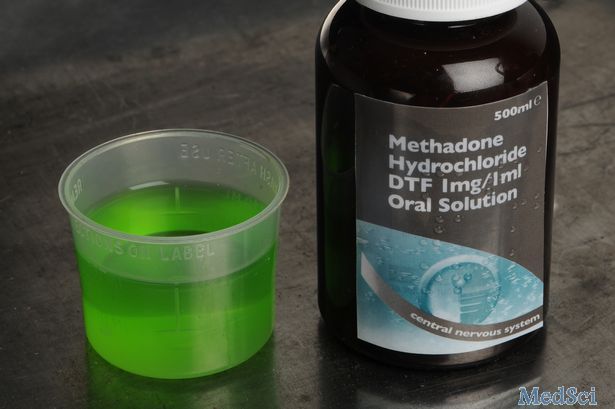
美沙酮和丁丙诺啡可降低阿片类药物过量后的死亡风险
2018-06-24 MedSci MedSci原创
美国国立卫生研究院(NIH)资助的一项研究发现,在非致命性阿片类药物过量使用后,美沙酮或丁丙诺啡治疗显著降低了阿片类药物相关死亡率。
美国国立卫生研究院(NIH)资助的一项研究发现,在非致命性阿片类药物过量使用后,美沙酮或丁丙诺啡治疗显著降低了阿片类药物相关死亡率。
研究者分析了马萨诸塞州17,568名成年人在2012年至2014年间阿片类药物过量使用后幸存的数据。与那些未接受药物辅助治疗的患者相比,接受美沙酮治疗的阿片类药物过量死亡人数减少了59%。但由于样本量较小,作者无法得出有关美沙酮的结论,并指出需要进一步对较大样本开展工作。丁丙诺啡、美沙酮和纳曲酮是FDA批准用于治疗阿片类药物使用障碍(OUD)的三种药物,这项研究是首次探究丁丙诺啡、美沙酮和纳曲酮与非致命性阿片类药物过量所导致的死亡率之间的关系,这项大样本研究证实了之前关于美沙酮和丁丙诺啡可以有效治疗OUD并预防死亡的结论。
尽管有令人信服的证据,尽管药物辅助治疗可以帮助许多人从阿片成瘾症中恢复过来,但这些已证实的药物仍然未被充分利用。该研究还发现,在服药过量后的第一年,只有不到三分之一的患者接受了药物治疗:美沙酮(11%)、丁丙诺啡(17%)、和纳曲酮(6%)。
原始出处:
https://www.europeanpharmaceuticalreview.com/news/76610/methadone-buprenorphine-opioid/
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#药物过量#
53
#阿片类药物#
0
#死亡风险#
53
#阿片类#
36
#美沙酮#
41
#丁丙诺啡#
40