Lung Cancer:Pembrolizumab+化疗对比 atezolizumab+化疗+/− 贝伐珠单抗一线治疗晚期非鳞状非小细胞肺癌(NSCLC)的疗效:匹配调整的间接比较分析
2021-07-13 yd2015 MedSci原创
pembrolizumab + 化疗较atezolizumab + 化疗能够带来OS和PFS获益,而较atezolizumab + 化疗+贝伐珠单抗带来PFS获益。
晚期非鳞状非小细胞肺癌(NSCLC)的标准治疗为免疫治疗联合化疗。但是目前没有头对头的研究对比哪一种免疫联合化疗疗效较好。因此,来自美国的研究团队进行了一项间接比较分析,比较Pembrolizumab+化疗对比 atezolizumab+化疗+/− 贝伐珠单抗一线治疗晚期非鳞状非小细胞肺癌(NSCLC)的疗效。相关研究发表在Lung Cancer杂志上。
研究患者主要为KEYNOTE-021 队列G (KN021 G) (pembrolizumab + 卡铂 +培美曲塞; N = 59) 和KEYNOTE-189 (KN189) (pembrolizumab + 培美曲塞 +铂类; N = 410) ,以及IMpower 130 (atezolizumab + 卡铂 + 白蛋白结合型紫杉醇; N =451) 和 IMpower 150 (atezolizumab + 卡铂 +紫杉醇 +贝伐珠单抗; N =356)。对两组的基线特征进行调整,然后评估调整后的OS,PFS和客观缓解率(ORR)。
经过对IMpower 130中atezolizumab+化疗患者的调整匹配,Pembrolizumab+化疗组有428例患者。pembrolizumab + 化疗对比atezolizumab +化疗的中位OS分别为23.0个月 [95 % CI: 19.8,25.8]和18.2个月 [95 % CI: 15.2, 20.3](HR=0.8,95%CI, 0.67,0.95)。中位PFS分别为9.3 个月 [95 % CI: 8.6, 11.1]和7.3个月 [95 % CI: 7.0, 8.6] (HR=0.79,95%CI, 0.67,0.93)。两组的6个月,1年和2年OS率分别为85.6 vs 79.8%,70.5 vs 62.2%,和 48.2 vs 40.0 %;而两组的6个月,1年和2年PFS率分别为69.3 vs 59.7%,42.6 vs 34.5%和26.3 vs 18.5 %。
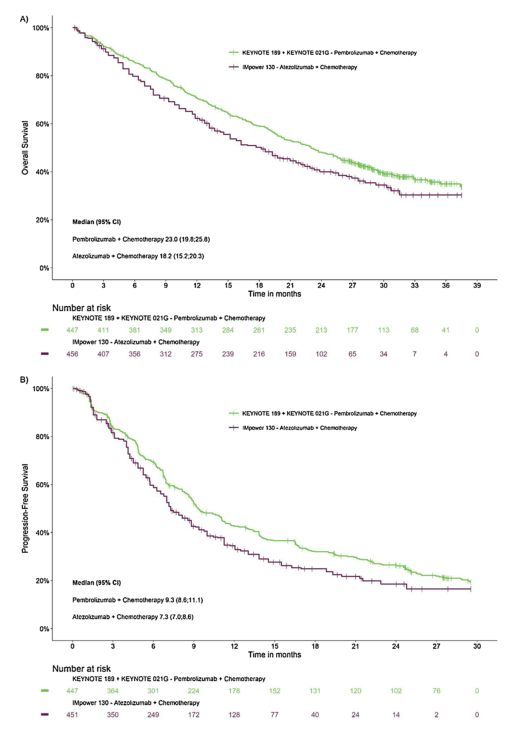
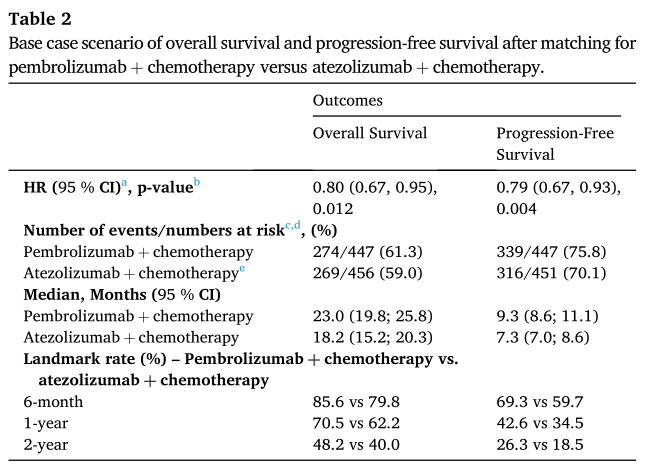
疗效对比1
经过对IMpower 150中atezolizumab+化疗+贝伐珠单抗患者的调整匹配,Pembrolizumab+化疗组有389例患者。pembrolizumab + 化疗对比atezolizumab +化疗+贝伐珠单抗的中位PFS分别为22.4个月和19.3个月(HR=0.86,95%CI, 0.72, 1.03)。中位PFS分别为9.2 个月和8.5个月 (HR=0.81,95%CI, 0.68, 0.96)。两组的6个月,1年和2年OS率分别为85.7 vs 84.0%,68.6 vs 67.1%,和 47.2 vs 41.6%;而两组的6个月,1年和2年PFS率分别为68.5 vs 64.4%,40.9 vs 36.7%和24.3 vs 7.6 %。
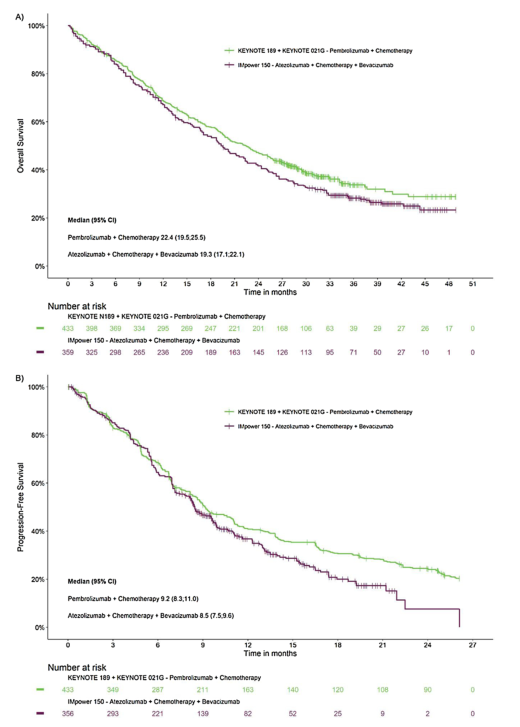
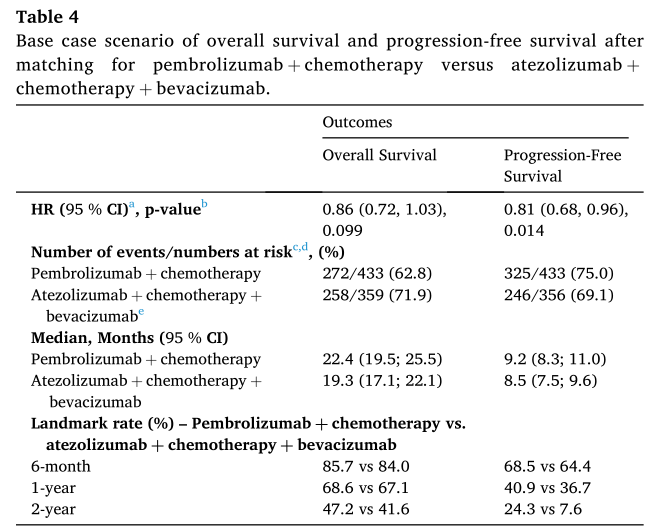
疗效对比2
对于ORR, pembrolizumab +化疗与atezolizumab +化疗的评估风险比(95% CI)和风险差异(95% CI)分别为0.9(0.8,1.1)和- 3.5%(-10.0,3.1)。而pembrolizumab +化疗与atezolizumab +化疗+贝伐珠单抗组分别为0.8(0.7,0.9)和- 12.2%(-19.6,-4.8)。
综上,研究表明, pembrolizumab + 化疗较atezolizumab + 化疗能够带来OS和PFS获益,而较atezolizumab + 化疗+贝伐珠单抗带来PFS获益。
原始出处:
Halmos B, Burke T, Kalyvas C, et al. Pembrolizumab+chemotherapy versus atezolizumab+chemotherapy+/-bevacizumab for the first-line treatment of non-squamous NSCLC: A matching-adjusted indirect comparison. Lung Cancer. 2021 May;155:175-182. doi: 10.1016/j.lungcan.2021.03.020. Epub 2021 Mar 30. PMID: 33839603.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
31
#非小细胞#
44
#贝伐珠#
45
#比较分析#
30
#mAb#
35
#Pembro#
36
#Pembrolizumab#
36
#非鳞状非小细胞肺癌#
36
#贝伐#
32
谢谢梅斯提供这么好的信息,学到很多
42