Arthritis Rheumatol:巨细胞动脉炎的诊断评估策略和疾病亚群
2019-11-25 xiangting MedSci原创
血管成像越来越多地被纳入GCA的诊断评估中,并根据颞动脉和颅外动脉受累来识别患者的临床亚群。
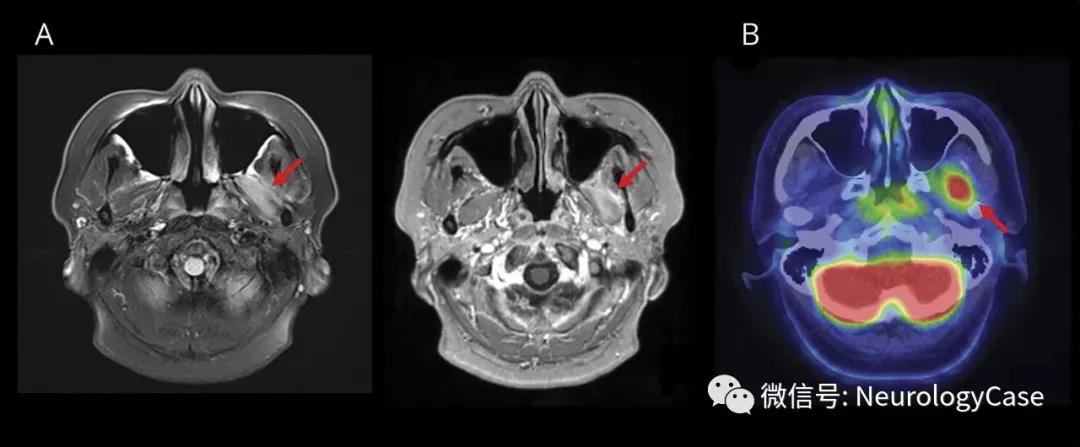
随着血管成像技术的日益普及,巨细胞动脉炎(GCA)的诊断评估正在迅速发生变化。这项研究目的是确定GCA的临床亚群是否具有不同的特征或反映不同的诊断评估。
从一个国际性队列中招募患者,并根据颞动脉(TA)异常[TA活检阳性(TAB)或TA超声的光晕征(TA-US)]和/或大血管(LV)受累的影像学证据将其分为四个亚群:1)TA异常和LV受累[TA(+)/LV(+)GCA];2)没有大血管受累的TA异常[TA(+)/LV(-)GCA];3)大血管受累,无TA异常[TA(-)/ LV(+)GCA];和4)临床诊断的GCA,无大血管受累或TA异常[TA(‐)/LV(‐)GCA]。
从72个国际研究中心招募了941名GCA患者。大多数患者进行了多种形式的诊断评估,包括TAB(n=704,75%);TA‐US(n=328,35%); 和LV成像(n=534,57%)。66%的TAB、79%的TA-US和40%的LV成像证实了GCA。GCA亚群具有不同的特征,与诊断评估策略无关。TA(+)/LV(-)是最常见的亚群(51%),颅脑缺血负担较高。TA(‐)/LV(‐)(26%)颅脑缺血和肌肉骨骼症状的患病率高。TA(‐)/LV(+)(12%)上肢血管异常多见,视力丧失患病率低。TA(+)/LV(+)(11%)的年龄较大,颅脑缺血、全身症状的患病率高和急性期反应物升高。
血管成像越来越多地被纳入GCA的诊断评估中,并根据颞动脉和颅外动脉受累来识别患者的临床亚群。
原始出处:
K.
Bates Gribbons. Diagnostic Assessment Strategies and Disease Subsets in Giant
Cell Arteritis: Data from an International Observational Cohort. Arthritis Rheumatol. 14 November 2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Arthritis#
31
#动脉炎#
38
#ART#
33
#巨细胞#
43