JACC:振奋人心——迟发型心肌梗死患者行PCI术仍能明显获益!
2021-09-23 MedSci原创 MedSci原创
晚期STEMI患者的冠状动脉血管重建与更好的短期和长期临床结果有关。
急性心肌梗死是由于灌注量与需求量长时间失衡而发生的心肌细胞坏死。 ST 段抬高型心肌梗死(STEMI)是指具有典型的缺血性胸痛,持续超过20分钟,血清心肌坏死标记物浓度升高并有动态演变,心电图具有典型的ST段抬高的一类急性心肌梗死。通常这类患者主要由冠状动脉出现完全动脉粥样硬化性阻塞所致。
由于STEMI是危及生命的急重症,因此STEMI的处理首先是快速识别,因为再灌注治疗只有在就诊后尽快进行才最有效。对于有胸痛且怀疑为急性冠脉综合征(ACS)的急诊科就诊患者,可用心电图确诊STEMI。生物标志物在早期可能正常。
经皮冠状动脉介入治疗(PCI)可减少ST段抬高型心肌梗死(STEMI)患者的梗死面积并改善结局。然而,高达50%的可行心肌的损失可能是由于再灌注损伤和相关的炎症反应造成的。通常将症状发生后12-48小时内出现的患者被归类为晚期患者。
目前有关STEMI患者在症状出现后晚期(>12小时)的最佳处理方法仍有争议。为了更好评估晚期STEMI患者的特征、时间趋势和血管再造的影响,来自法国图卢兹Rangueil大学医院心脏外科的专家分析了FAST-MI(法国急性ST段抬高和非ST段抬高心肌梗死登记处)项目的3项全国性观察研究的数据,结果发表在近期JACC杂志上。
结果3个队列中共有6273名STEMI患者,其中1169人(18.6%)是迟发型患者。在排除了接受纤维蛋白溶解治疗的患者和入院后2天内死亡的患者后,分析了1077名患者,其中729名(67.7%)在入院后48小时内进行了血管重建(PCI术)。
在30天的随访中,晚期接受血管重建的患者的全因死亡率明显降低(2.1% vs 7.2%;P < 0.001)。在58个月的中位随访后,血管重建晚期患者组的全因死亡率为30.4/1000人年(95%CI:25.7-35.9),而非血管重建晚期患者组为78.7/1000人年(95%CI:67.2-92.3)(P<0.001),可见患者仍能从长期随访中获益。
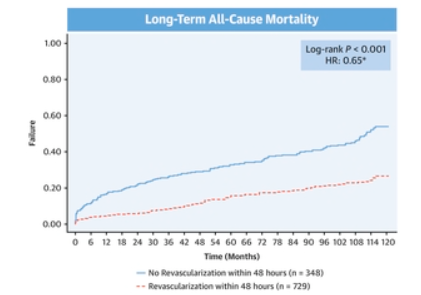
两组患者在长期随访中全因死亡率的差异
此外,在多变量分析中,晚期STEMI患者的血管重建与随访期间死亡发生率降低35%有关(HR=0.65 [95% CI:0.50-0.84];P = 0.001)。
综上,晚期STEMI患者的冠状动脉血管重建与更好的短期和长期临床结果有关。
参考文献:
Percutaneous Myocardial Revascularization in Late-Presenting Patients With STEMI. J Am Coll Cardiol. 2021 Sep, 78 (13) 1291–1305
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#迟发型#
62
#JACC#
45
#PCI术#
56
好的
0
#ACC#
48
已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读
0