Circulation:该睡不睡,心脏遭罪!我国学者发现打破昼夜节律致心脏病的机制
2022-01-19 医诺维 医诺维
昼夜节律,即生物钟,已得到科学家的广泛研究。昼夜节律赋予了人类行为和生理学的时间模式,使身体内在与外在环境的预期变化保持一致,被扰乱的昼夜节律会对健康产生影响。逆天而行的作息会增加代谢紊乱的风险。
昼夜节律,即生物钟,已得到科学家的广泛研究。昼夜节律赋予了人类行为和生理学的时间模式,使身体内在与外在环境的预期变化保持一致,被扰乱的昼夜节律会对健康产生影响。逆天而行的作息会增加代谢紊乱的风险,从代谢和心血管疾病的风险增加到精神疾病和癌症。
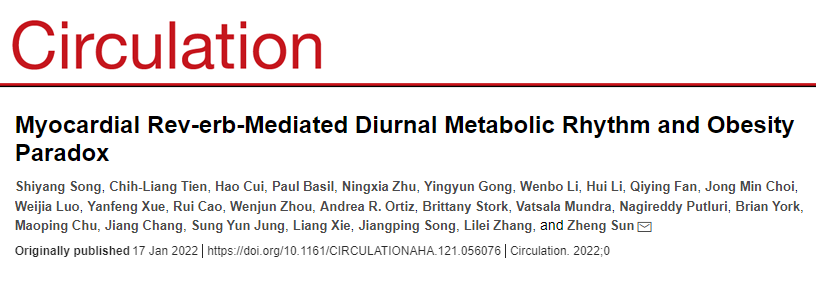
2022年1月17日,中国医学科学院心血管疾病研究中心和北京协和医学院、贝勒医学院等研究人员在《美国心脏学会》旗下" Circulation "期刊上发表了一篇题为" Myocardial Rev-erb-Mediated Diurnal Metabolic Rhythm and Obesity Paradox "的研究论文。
该研究表明,在睡眠期间和白天活动期间,心脏的代谢以不同的能量来源供给。心肌细胞中的Rev-erbα/β调控正常的代谢节律,去除Rev-erbα/β会破坏这种节律,降低心肌细胞在睡眠期间使用脂质的能力,导致进行性扩张型心肌病和致命的心力衰竭。
在该研究中,研究人员分析了小鼠清醒和睡眠期间的基因和蛋白表达,以及一组全面的代谢物和脂质,发现Rev-erbα/β基因仅在睡眠时间内高度表达,其活性与脂肪和糖代谢有关。
对此,研究人员猜测,当Rev-erbα/β敲除,心脏在睡眠期间不能有效利用脂肪酸时,就没有足够的能量维持跳动,从而导致进行性扩张性心肌病。
为了验证这一猜测,研究人员分析了敲除Rev-erbα/β的小鼠,通过对心肌细胞的分析发现,敲除Rev-erbα/β的小鼠在睡眠期间降低了脂肪利用率,相反,提高了糖的利用率。
结果表明,在睡眠阶段,心脏利用脂肪释放的脂肪酸作为主要的能量来源,敲除Rev-erbα/β,心脏会有代谢缺陷,在睡眠期间限制脂肪酸的使用,而在活动阶段会过度使用糖。
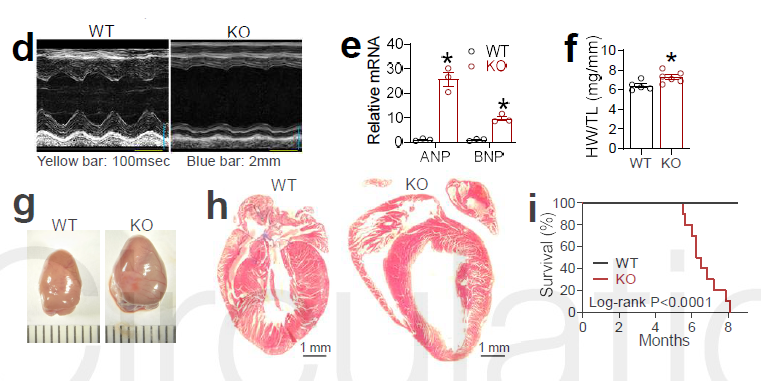
敲除Rev-erbα/β可导致致命性心力衰竭
接下来,研究人员又分析了补充脂肪酸是否会改善这种情况。
研究人员给Rev-erbα/β基因敲除的两组小鼠分别喂食高脂肪食物。一组喂食高脂肪,另一组喂食高蔗糖饮食,类似于促进肥胖的人类饮食。
研究发现,高蔗糖饮食在一定程度上缓解了心脏缺陷,但高脂肪饮食没有。
研究表明,心肌细胞中的Rev-erbα/β调控正常的代谢节律,在动物的睡眠期间,心脏以脂质作为能量来源。去除Rev-erbα/β会破坏这种节律,降低心肌细胞在睡眠期间使用脂质的能力,导致进行性扩张型心肌病和致命的心力衰竭。
重要的是,研究还表明,纠正代谢缺陷有助于改善病情。

高蔗糖饮食缓解了心脏缺陷
研究人员表示,这项研究具有三个临床意义。
首先,发现心脏昼夜节律与心脏扩张的严重程度相关。
第二,肥胖和胰岛素抵抗,这两个长期被认为是导致心力衰竭的临床危险因素,却可以起到保护作用。
最后,通过药物控制脂肪酸和糖代谢可以改善病情,但重要的是给药与相应代谢途径的内在昼夜节律一致。
研究人员强调,该研究突出了时间疗法的重要性,即根据昼夜节律安排药物治疗,不仅在这项研究中如此,对许多其他药物也是如此,在安排用药时将昼夜节律考虑在内是非常重要的。
原始出处:
Shiyang Song , Chih-Liang Tien , Hao Cui, et al. Myocardial Rev-erb-Mediated Diurnal Metabolic Rhythm and Obesity Paradox. Circulation. 2022;0.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#我国学者#
49
以后不敢熬夜了
52
学习#学习#
51
学习了,谢谢分享
45
what
51