ACC 2020:TAVR对二叶式主动脉瓣治疗效果良好
2020-04-05 MedSci MedSci原创
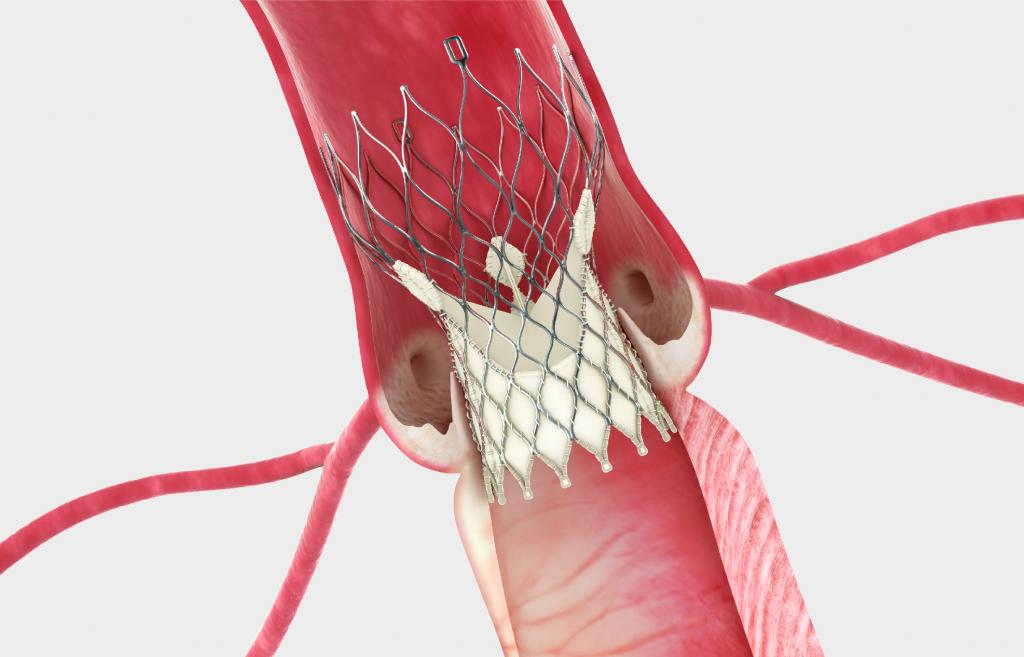
根据在ACC.20/WCC中公布的一项最新临床试验结果,经导管主动脉瓣置换术(TAVR)手术对二叶式主动脉瓣(BAV)的成功率很高,患者30天内死亡或致残的风险较低。
根据在ACC.20/WCC中公布的一项最新临床试验结果,经导管主动脉瓣置换术(TAVR)手术对二叶式主动脉瓣(BAV)的成功率很高,患者30天内死亡或致残的风险较低。
这项名为Evolut Low Risk Bicuspid Study是第一项前瞻性观察相对年轻健康的严重主动脉狭窄患者置入双尖瓣治疗,这也第一个研究使用自膨胀人工瓣膜TAVR治疗严重主动脉瓣狭窄患者的研究。
该研究的共同研究者Basel Ramlawi博士说:“在低风险的二叶式主动脉瓣患者中,使用自膨胀人工瓣膜是一种非常可行和安全的方法,并且取得了很好的早期效果。”“尽管有必要进行进一步的随访,以确定长期的结果,但早期的结果表明,这一过程可以在低风险人群中成功地进行,并取得良好的结果。”
该研究前瞻性地追踪了在美国25个医疗中心接受TAVR治疗的150名患者,平均年龄为70岁,并且胸科医师协会评分(Society of Thoracic Surgeons risk score)为1.4%。在手术30天后,1.3%的病人死亡或发生过致残性卒中,这是该研究的主要安全性终点。
患者的治疗成功率为95.3%,这说明主要并发症、瓣膜不合适或需要额外的手术的发生率低。绝大多数(99.3%)的病人在手术中存活了下来,96%的病人实现了正确的瓣膜定位,100%的病人有轻微的或没有主动脉回流。
在有西弗斯型0型瓣膜(Sievers type 0 valve)的病人中,84.6%的病人有追踪或没有主动脉回流,其余的只有轻微的漏泄,Ramlawi说这是一个很高的成功率,这在某种程度上是意料之外的,因为在这种形状的瓣膜上操作很复杂。
除了没有随机对照之外,研究人员还指出,这项研究是在医疗中心进行的,这些医疗中心有大量的TAVR手术,在经验较少的中心是否会得到类似的结果尚不清楚。Ramlawi说:“这是第一个表明自扩张瓣膜对1型和0型二叶式主动脉瓣病人都有效的研究。医学界已经认为,0型双尖瓣更具有挑战性,因此这些数据尤其令人鼓舞。”
关于TAVR手术
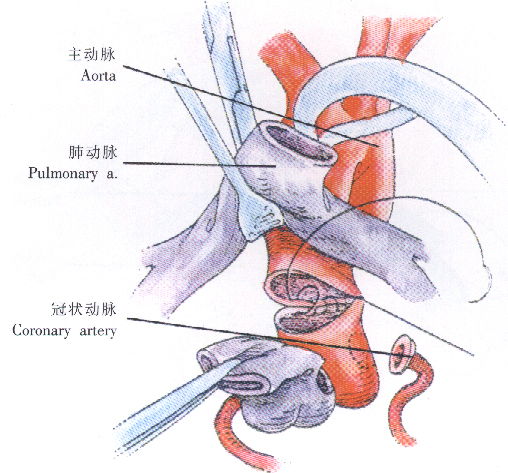
2002年,Alain Cribier博士和同事们在法国鲁昂大学Charles Nicolle大学医院完成了首例经导管主动脉瓣置换术(TAVR)。15年来,TAVR发展迅速,带来了心血管医学领域的巨大变革。TAVR成为主动脉瓣狭窄患者的治疗新选择,显著改善了严重主动脉瓣狭窄患者的生活质量。
瑞士伯尔尼大学医院心脏科前任主任Bernhard Meier博士说,TAVR是除了冠状动脉成形术之外的最重要的经导管心脏介入治疗……它将完全取代孤立的退行性主动脉瓣外科置换术。
在TAVR出现之前,很多严重主动瓣膜狭窄患者的选择是有限的。外科主动脉瓣置入术(SAVR)被认为是最好的选择,但大部分患者的手术风险太高。有些患者进行球囊瓣膜成形术是有效的,但通常效果不能持久。
ACC前任主席、梅奥诊所的David R. Holmes Jr.教授介绍,球囊主动脉瓣成形术并不能满足大多数患者的临床需求,因此,开发基于导管的替代瓣膜手术引起了研究者的极大兴趣。经过长期发展,2002年,Cribier博士引入了TAVR。
十多年来,TAVR在临床的使用大幅增加,其适应证不断扩展。2011年,FDA首次批准了TAVR系统——一种球囊扩张瓣膜(Sapien)。在此之前,TAVR技术已经在40多个国家获得批准。2014年出现了一种自膨胀瓣膜,即CoreValve。
最初,这两种系统被批准用于无法手术或有手术极高危的患者;后来,其适应证扩展到手术高危患者;再后来,扩展到中危患者。两种系统都经历了多代更新,目前正在低危患者中进行测试。目前FDA正在审查第三种TAVR系统——Lotus。
目前,在美国开展的经导管瓣膜治疗(TVT)注册研究已经纳入了9万多名患者。该研究不断发布新的数据。未来,TVT注册研究将继续提供有关美国TAVR演进的有意义的信息。随着技术进步和手术流程简化,未来十年,TAVR的数量仍将有惊人的增长。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#治疗效果#
34
#AVR#
0
#二叶式主动脉瓣#
38
#ACC 2020#
41
#ACC#
33
#主动脉瓣#
22
#主动脉#
28
谢谢梅斯提供这么好的信息,学到很多
58
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
57