Circulation:美国TAVR注册研究报告:介入治疗二叶式主动脉瓣狭窄的效果与三叶式瓣膜相当
2020-02-28 朱朱 中国循环杂志
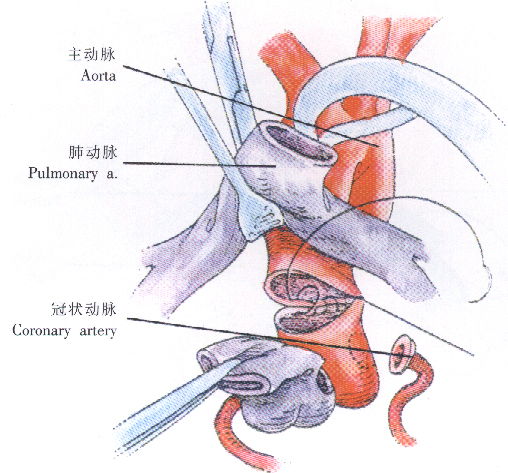
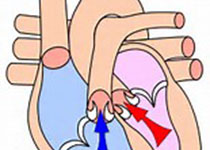
二叶式主动脉瓣由于其特殊的解剖结构及力学表现,尤其是0型二叶瓣,行经导管主动脉瓣置换(TAVR)术易发生瓣周漏、瓣膜移位、主动脉夹层等并发证,其手术难度和风险均高于三叶式主动脉瓣。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#研究报告#
29
#AVR#
0
#注册研究#
39
#二叶式主动脉瓣#
32
#主动脉瓣#
32
#主动脉#
21
#注册#
25
#瓣膜#
24
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
40