Int J Rheum Dis:长期随访结果表明手术仍然是强直性脊柱炎患者AL的更佳治疗方法
2021-05-04 MedSci原创 MedSci原创
强直性脊柱炎(AS)是一种众所周知的慢性炎症性风湿病,会导致脊柱结构的渐进性损伤和运动受限。Andersson病变(AL)是AS患者的罕见并发症,表现为脊柱的破坏性椎体或发现性椎体病变。大多数关于AL
强直性脊柱炎(AS)是一种众所周知的慢性炎症性风湿病,会导致脊柱结构的渐进性损伤和运动受限。Andersson病变(AL)是AS患者的罕见并发症,表现为脊柱的破坏性椎体或发现性椎体病变。大多数关于AL的临床研究都是基于病例报告和小样本的回顾性研究,所以缺乏对这种病变的中长期结果的大规模调查。近日,研究人员利用中长期随访数据评估了AL治疗的临床疗效和预后因素,并探讨了AL的临床特点和治疗方法,研究结果已发表于Int J Rheum Dis。

2011年6月至2018年3月,研究人员对48例连续AL病例进行了回顾性分析,包括13例保守治疗和35例手术治疗。回顾了流行病学特征、治疗方式、临床特征和结果,以及日本骨科协会(JOA)康复率的预后因素。通过美国脊柱损伤协会(ASIA)的分类进行评估患者神经功能的恢复。由JOA评分、视觉模拟量表(VAS)评分和Cobb角度来评价临床疗效。
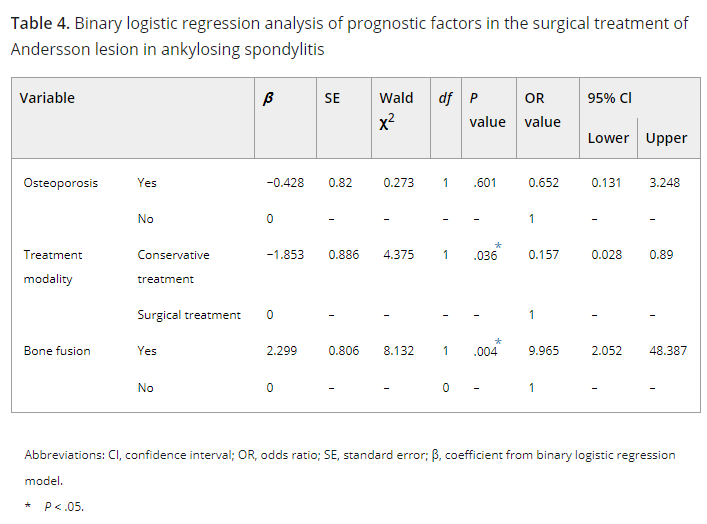
结果,平均总体随访时间为(44.5±18.5)个月(范围为27-85个月)。36名男性和12名女性患者,平均年龄为49.4±13.1岁(范围,26-72岁)。最常见的病变位置是胸腰部,即T10-L2(n=33;68.8%),其次是胸椎(n=10)和腰椎(n=5)。在最后的随访中,手术治疗的患者的JOA评分、VAS评分和Cobb's角度都明显优于保守治疗的患者(P<.05)。单变量和二元逻辑回归分析确定了影响JOA评分恢复率的两个预后因素:治疗方式(OR=0.157;95%CI,0.028-0.89;P=0.036)和骨融合(OR=9.965;95%CI,2.052-48.387;P=0.004)。保守治疗和骨不连预示着更差的JOA评分恢复。
综上所述,该研究结果表明,手术仍然是强直性脊柱炎患者AL的最佳治疗方法,中长期随访数据证明了其更好的临床疗效。
原始出处:
Minhao Wu, et al., Effects of Andersson lesion treatment in ankylosing spondylitis: A medical record review study focused on medium- to long-term outcomes. Int J Rheum Dis. 2020 Jun;23(6):753-762. doi: 10.1111/1756-185X.13826.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#随访结果#
54
#强直性#
44
#Dis#
28
#长期随访#
48
受益匪浅#学习#
84
#治疗方法#
51
#脊柱炎#
34