肿瘤脑转移(Brain metastases,BrM)影响着20-40%的实体恶性肿瘤患者,并与重大的临床后遗症有关,包括癫痫发作。癫痫发作是大约10-20%患者被诊断为BrM的的一个表现症状,尽管根据以前的研究,对这一估计数字各有不同。对于出现癫痫发作的患者,应开始服用抗癫痫药物(antiseizure medication,ASM),以减少进一步发作的发展。在BrM诊断时未出现癫痫发作的患者中,随后癫痫发作的发生率仍然描述得很模糊。虽然目前的指南并不推荐在癫痫病人诊断为BrM后开始ASM,但这种指南主要是基于数量有限的、小型的单中心研究,他们的研究样本量小、而队列异质性高,这些研究并没有显示出接受ASMs与不接受ASMs的患者的癫痫发作风险显著降低。
此外,越来越多地使用与晚期炎症或坏死相关的治疗方法,如立体定向放疗和免疫治疗,可能会增加当代队列中的癫痫发作风险。癫痫发作的发生有可能对患者的生活质量造成极大的损害,因为癫痫发作患者的活动会受到限制;通常癫痫发作往往会引起急诊科的就诊,而如果利用预防性的ASMs,就有可能避免这种情况,这对患者和医疗系统都很受益。因此,有必要重新考虑在当下的治疗中,对部分BrM患者中预先使用ASMs。
藉此,哈佛大学的Nayan Lamba等人,探究了尚未表现为癫痫发作的肿瘤脑转移(BrM)患者, 后来癫痫发作的风险是否会增加,并分析了相应的癫痫发作的发生率和危险因素。
他们利用监测、流行病学和最终结果(SEER)-Medicare数据(2008-2016年)和Brigham and Women’s
Hospital/Dana Farber Cancer Institute(2000-2015年)机构数据,分别纳入了15863名和1453名BrM患者。通过累积发生率曲线和Fine/Gray的竞争风险回归描述癫痫发作发生率和风险因素。
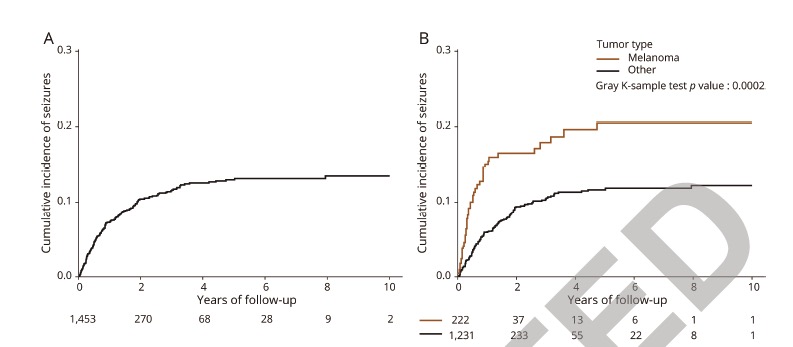
结果显示,在SEER-Medicare和机构患者中,分别有1588人(10.0%)和169人(11.6%)出现癫痫发作。在SEER-Medicare队列的中,癫痫发作风险相关因素包括: 非裔美国人vs白人种族(HR=1.45),城市vs非城市居住地(HR=1.41)、黑色素瘤vs.非小细胞肺癌(HR=1.44 )、接受脑部定向立体定向辐射(HR=1.67 )。
在机构队列中,黑色素瘤与非小细胞肺癌(HR=1.70 )、诊断时大于4个BrM(HR=1.60 )、高危位置存在BrM(HR=3. 62 ),缺乏局部脑导向治疗(HR=3.08 )与癫痫发作发展的风险更大有关。
这个研究的重要意义在于,对于部分BrM患者中,,特别是患有黑色素瘤、颅内疾病负担较大、BrM在高危部位的患者,可以适当应用抗癫痫药物。
原文出处
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Neurol#
38
已看,还可以。
60
#脑转移患者#
50
学习了,谢谢分享
100
获益匪浅
102
#肿瘤脑转移#
96
说得很好,确实临床获益
94