Neurology:见于卡培他滨诱发脑白质病的短暂性缄默伴胼胝体压部病变
2019-03-30 zyx整理 神经科病例撷英拾粹
50岁女性,在卡培他滨(1250mg/m2,每天两次)治疗进展期胃癌第7天,出现反复发作性缄默。发作间期神经系统查体提示轻度左侧偏瘫和右侧巴氏征。
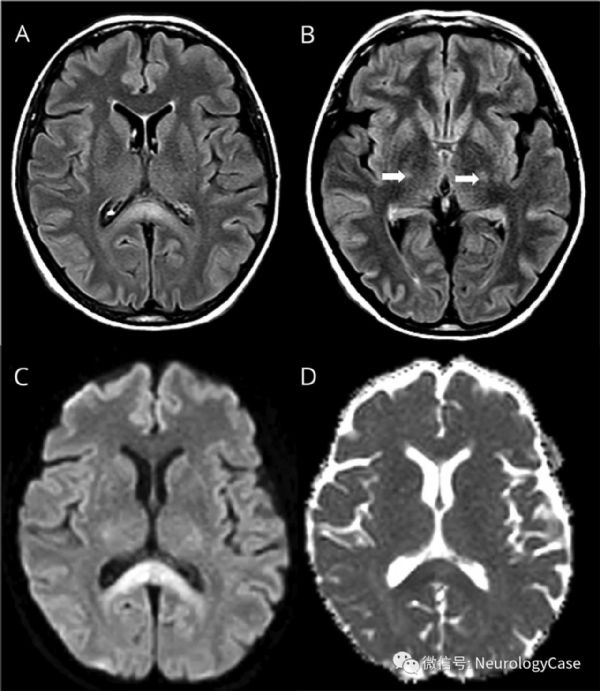
50岁女性,在卡培他滨(1250mg/m2,每天两次)治疗进展期胃癌第7天,出现反复发作性缄默。发作间期神经系统查体提示轻度左侧偏瘫和右侧巴氏征。脑CT,发作期脑电图,电解质,血氨,维生素B1和B12检测均无明显异常。脑MRI可见胼胝体压部和皮质脊髓束DWI和FLAIR上双侧对称高信号(图)。停用化疗药后2天症状好转。在耐药性癫痫行胼胝体切开术后和通常累及胼胝体纤维的中毒性白质脑病患者中已有短暂性缄默的报道。
(图:FLAIR可见胼胝体[A]和皮质脊髓束[B,箭]双侧对称高信号;DWI[C]和ADC[D]序列可见弥散受限,符合细胞毒性水肿,提示急性中毒性白质脑病)
原始出处:Nicoletti T, Spagni G, Luigetti M, Iorio R. Teaching NeuroImages: Transient mutism associated with splenium lesion in capecitabine-induced leukoencephalopathy. Neurology. 2019 Feb 26;92(9):e1000-e1001.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#白质#
38
#Neurol#
38
#胼胝体压部#
45
#短暂性#
30
#胼胝体#
35
#卡培他滨#
24
#脑白质病#
32