Nature:较低的促进癌细胞扩散和转移
2022-05-31 生物谷 生物谷
当肿瘤减少PHGDH的丰度时,其他酶和它们协调的过程就会步入正轨。就TNBC而言,一个结果是产生了唾液酸。这种酸帮助癌细胞在转移过程中粘附在其他细胞和生物组织成分上。
在一项新的研究中,来自比利时鲁汶大学、荷兰癌症研究所、加拿大麦吉尔大学、德国癌症研究中心和美国密歇根州立大学等研究机构的研究人员揭示了人某种形式的转移性乳腺癌---三阴性乳腺癌(TNBC)---如何扩散到身体的其他部位的分子机制。通过这样做,他们为发现和遏制三阴性乳腺癌带来了新机会。相关研究结果发表在2022年5月26日的Nature期刊上,论文标题为“PHGDH heterogeneity potentiates cancer cell dissemination and metastasis”。

论文共同作者、密歇根州立大学自然科学学院副教授Sophia Lunt说,“我们专注于TNBC,因为它在年轻患者中发生的比例更高,而且临床结果更差。”
Lunt说,“绝大多数与TNBC有关的死亡是由于转移,即癌细胞从原发肿瘤扩散到身体的其他部位。转移性乳腺癌是无法治愈的,现有的治疗方法仅旨在减缓疾病进展。”
自2015年加入密歇根州立大学以来,Lunt的研究重点是了解代谢---癌细胞使用哪些营养物和化合物以及如何它们---在转移中发挥作用。她和她的团队如今报告了他们对TNBC的研究结果,TNBC之所以被命名是因为它的肿瘤细胞对用于诊断的三种类型的蛋白检测为阴性。
在这篇论文中,这些作者发现磷酸甘油酸脱氢酶(phosphoglycerate dehydrogenase, PHGDH)水平低的癌细胞构成了更大的扩散风险。Lunt说,这个结果一开始令人惊讶,因为癌细胞也使用这种酶来增殖。肿瘤中的这种酶越多,它就越有可能生长。然而,较低的PHGDH水平有助于肿瘤的扩散。这一发现得到了来自人类乳腺癌患者的数据以及对癌细胞和小鼠模型的额外研究的支持。
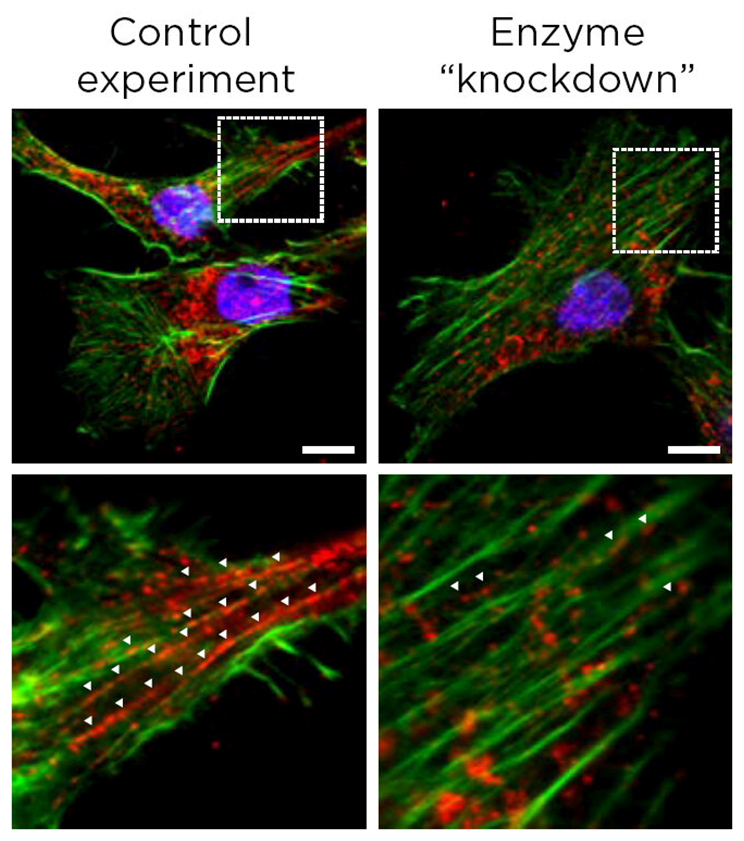
这些荧光显微图图片有助于说明级联效应如何导致癌细胞转移。图片来自Nature, 2022, doi:10.1038/s41586-022-04758-2。
Lunt说,“我们最初预计PHGDH的高表达会支持增殖和转移。然而,这一结果是有意义的,因为癌细胞在增殖和转移期间的需求是非常不同的。在增殖期间,癌细胞希望在熟悉的环境中尽可能快地进行分裂。在转移过程中,癌细胞必须在离开原发部位、通过血液流动、寻找新的部位并在一个陌生的环境中生存这一极其紧张的过程中生存下来。”
当肿瘤减少PHGDH的丰度时,其他酶和它们协调的过程就会步入正轨。就TNBC而言,一个结果是产生了唾液酸。这种酸帮助癌细胞在转移过程中粘附在其他细胞和生物组织成分上。
探究支撑这一系列反应和相互作用的分子机制是Lunt正在进行的研究的目标。破解癌症错综复杂的生物化学特性是具有挑战性的,但是全球合作有望克服这一领域的障碍。
Lunt说,“我们的研究可能导致新的生物标志物---比如低PHGDH和较高的唾液酸--来确定转移风险,并为转移性TNBC患者提供新的治疗靶标。”
参考资料:
Matteo Rossi et al. PHGDH heterogeneity potentiates cancer cell dissemination and metastasis. Nature, 2022, doi:10.1038/s41586-022-04758-2.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
39
很有意义
28
#癌细胞扩散#
34
#癌细胞#
57