JCO:NRG1融合阳性肺癌的临床病理特征和对各种治疗的反应性
2021-06-07 Nebula MedSci原创
NRG1基因融合阳性肺癌采用细胞毒性、免疫治疗和靶向治疗的疗效均较差
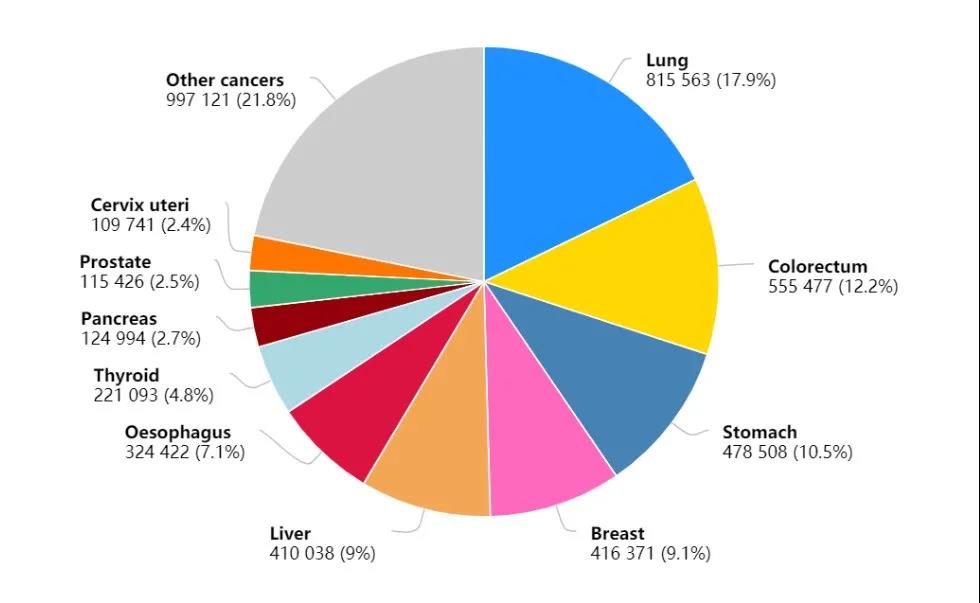
虽然NRG1基因融合是包括肺癌在内的多种类型肿瘤的致癌驱动因素,但由于其较为罕见,导致难以对其进行研究。因此建立了全球 eNRGy1 登记处,以在迄今为止最大和最多样化的系列中表征 NRG1基因融合阳性的肺癌。
从2018年6月至2020年2月,来自欧洲、亚组和美国的9个国家的22个中心组成的联盟提供了经病理验证的携带NRG1基因融合的肺癌患者的数据,包括以DNA和或RNA为基础的二代测序数据以及荧光原位杂交。并对临床、病理、分子和缓解(RECIST v1.1) 数据进行集中管理和分析。
共收录了110例NRG1融合阳性的肺癌患者,虽然典型的从不吸烟(57%)、粘液腺癌(57%)和非转移性(71%)表型占据了主导地位,但进一步的多样性,包括吸烟史(43%)和组织学(43%非粘液腺癌和6%非腺癌),也已被阐明。
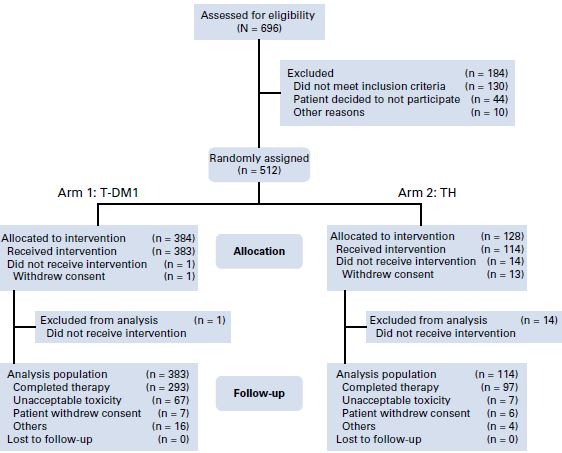
研究流程
以RNA为基础的检测鉴定出了大部分融合(74%)。在分子上,还发现了 6 个(共 18 个)新型5'端融合、20 个独特的表皮生长因子结构域 - 包含嵌合事件和异质性5'/3'端断点。
NRG1融合阳性的肺癌患者采用含铂双药和以紫杉醇为基础(在铂双药治疗后)的化疗治疗后的客观缓解率较低(ORRs分别是13%和14%),中位无进展生存期一般(PFS分别是5.8和4.0个月)。
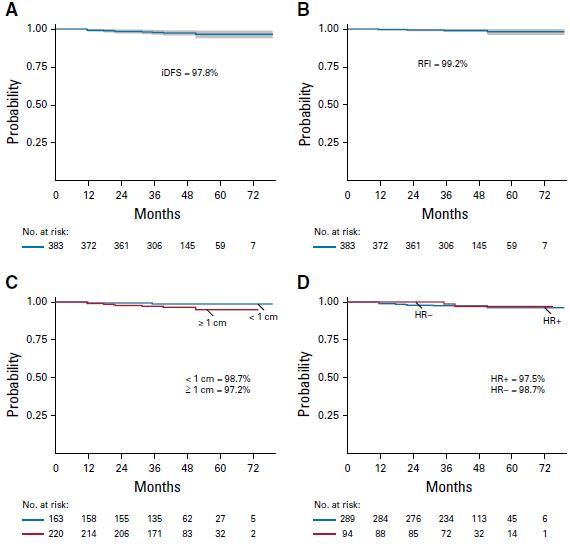
采用曲妥珠单抗治疗的患者预后
与低PD-L1表达(28%)和低肿瘤突变负荷(中位值 0.9个突变/Mb)免疫表型一致,这类患者采用化疗-免疫疗法和单免疫疗法治疗的活性较差(ORR分别为0%和20%,PFS分别为3.3和3.6个月)。采用阿法替尼治疗的ORR为25%,中位PFS为2.8个月。
总而言之,NRG1基因融合阳性肺癌在分子、病理和临床上比既往认识到的更具异质性。细胞毒性、免疫治疗和靶向治疗的活性均差强人意。未来需进一步研究NRG1重排的肿瘤生物学,以开发新的治疗策略。
原始出处:
Drilon Alexander,Duruisseaux Michael,Han Ji-Youn et al. NRG1Clinicopathologic Features and Response to Therapy of Fusion-Driven Lung Cancers: The eNRGy1 Global Multicenter Registry.[J] .J Clin Oncol, 2021, undefined: JCO2003307.https://doi.org/10.1200/JCO.20.03307
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#病理特征#
36
#JCO#
35
#临床病理#
47
#反应性#
47
#融合#
25