肺叶切除术后病人行神经外科坐位手术时发生疑似空气栓塞的围术期处理
2019-06-24 冯丹丹 张娟 马正良 实用老年医学
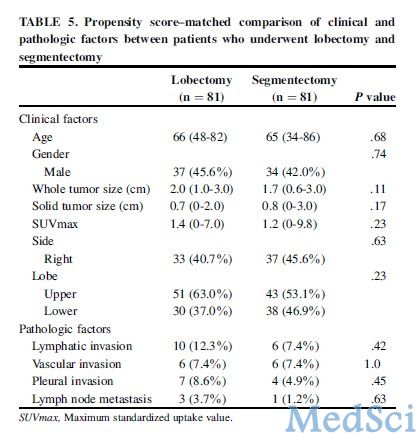
男,76岁,体质量83kg,因“右侧肢体活动障碍9月余”入院,入院诊断:1、颅内占位;2、左上肺腺癌;3、左上肺切除术后;4、前列腺增生。拟在全身麻醉下行开颅探查+占位切除并视情况行去骨瓣减压术,既往因左上肺腺癌行左上肺切除术。神清,听诊左上肺无呼吸音,左下肺、右肺呼吸音粗。全胸片:左胸术后改变,左侧胸腔黏连。肺功能:中度混合性通气功能障碍。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#围术期处理#
45
#切除术#
28
#围术期#
33
#肺叶切除#
51
666
78