EUR J Cancer:用以晚期实体瘤患者治疗的选择性MET酪氨酸激酶抑制剂SAR125844的I期临床
2017-12-26 MedSci MedSci原创
EUR J Cancer<span lang="ZH-CN" style="font-family:DengXian;mso-ascii-font-family:"Times New Roman";mso-fareast-font-family: DengXian;mso-fareast-theme-font:minor-fareast;mso-hansi-font-fam
EUR
J Cancer:用以晚期实体瘤患者治疗的选择性MET酪氨酸激酶抑制剂SAR125844的I期临床
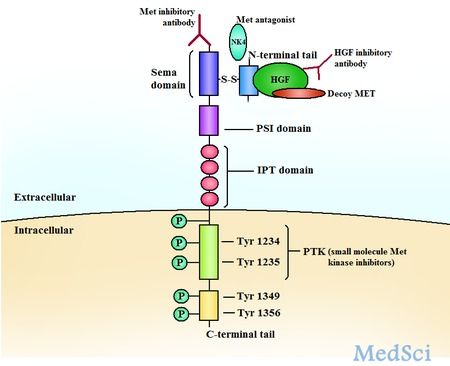
原癌基因MET编码了酪氨酸激酶受体MET,该受体能够结合肝细胞生长因子(HGF)。MET能够通过配体依赖性或非依赖性的方式参与肿瘤发生和许多癌症进程,并涉及到肿瘤的耐药性。研究人员对高度选择性的MET激酶抑制剂(SAR125844)的安全性和有效性在晚期实体瘤和MET失调的患者中进行了详细研究。
在试验中,通过免疫组化(IHC)或通过荧光原位杂交方法,证明了入组患者具有较高的总MET(t-MET)和磷酸化的MET(p-MET)表达水平。而该临床试验的目的为确定每周一次静脉注射SAR125844的最大耐受剂量(MTD)、安全性和药代动力学特征。
结果显示,最常见的治疗相关的不良反应事件(AEs)为乏力(58.3%),恶心(31.9%),腹痛,便秘和呼吸困难(各占27.8%);58.3%的患者报告有3级AE(19.4%为治疗相关)。每周一次SAR125844的MTD为570 mg/m2,SAR125844在MET扩增的非小细胞肺癌患者中具有显著的抗肿瘤活性。
原始出处:
Angevin, Eric,
et al. "A first-in-human phase I study of SAR125844, a selective MET
tyrosine kinase inhibitor, in patients with advanced solid tumours with MET
amplification." European Journal of Cancer 2017 87: 131-139. doi.org/10.1016/j.ejca.
本文系梅斯医学(MedSci)原创编译整理,转载需授权
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#激酶抑制剂#
25
#I期临床#
34
#选择性#
32
#酪氨酸激酶#
36
#MET#
32
#抑制剂#
26
#晚期实体瘤#
0
#激酶#
31