Radiology:人工智能技术在x线片骨折识别中的应用
2022-01-20 shaosai MedSci原创
在各种临床环境下,使用x线片明确骨折的存在是影像科最常见的工作之一。骨折的漏诊在影像科十分常见,这将延误患者的治疗,甚至造成严重的临床后果。因此,对骨折的准确识别及判断对临床至关重要。
 在各种临床环境下,使用x线片明确骨折的存在是影像科最常见的工作之一。骨折的漏诊在影像科十分常见,这将延误患者的治疗,甚至造成严重的临床后果。因此,对骨折的准确识别及判断对临床至关重要。
在各种临床环境下,使用x线片明确骨折的存在是影像科最常见的工作之一。骨折的漏诊在影像科十分常见,这将延误患者的治疗,甚至造成严重的临床后果。因此,对骨折的准确识别及判断对临床至关重要。
迄今为止,关于人工智能(AI)辅助骨折检测的几项研究只针对部分身体部位,且x线片的阅读者只针对了影像科医生和骨科医生,结果并不具有代表性。
近日,发表在Radiology杂志的一项研究评估了人工智能的协助对医生在X线片上骨折诊断表现的影响,为骨折的快速、准确诊断提供了支持。
本项回顾性诊断研究采用了多读取器、多案例的方法,基于2020年7月至2021年1月期间480次检查的外部多中心数据集,每个身体区域(脚和踝、膝和腿、髋和骨盆、手和手腕、肘和臂、肩和锁骨、肋骨和胸腰椎)至少有60次检查。骨折的发生率被设定为50%。基础真理由两位肌肉骨骼放射科医生确定,差异由第三位医生解决。向24名读者(放射科医生、骨科医生、急诊医生、助理医生、风湿病医生、家庭医生)展示了整个验证数据集(n = 480)。主要分析必须证明在人工智能的帮助下,每个患者的诊断敏感性有优势,每个患者的特异性在-3%的范围内没有劣势。独立的人工智能性能也使用受试者工作特性曲线进行评估。
共纳入480名患者(平均年龄,59岁±16[标准差];327名女性)。使用人工智能辅助工具(5760个读数中的4331个,75.2%)比不使用人工智能(5760个读数中的3732个,64.8%)的情况下,每位患者的敏感性提高10.4%(95% CI:6.9,13.9;P < .001为优)。有AI辅助的每位患者的特异性(5760次读数中的5504次,95.6%)不逊于无AI辅助的患者(5760次读数中的5217次,90.6%),差异为+5.0%(95%CI:+2.0,+8.0;P = .001为非劣质性)。AI使每次检查的平均读数时间缩短了6.3秒(95%CI:-12.5,-0.1;P = .046)。按病人增益的敏感性在所有区域都很明显(+8.0%至+16.2%;P < .05),但肩和锁骨以及脊柱(+4.2%和+2.6%;P = .12和.52)并不明显。

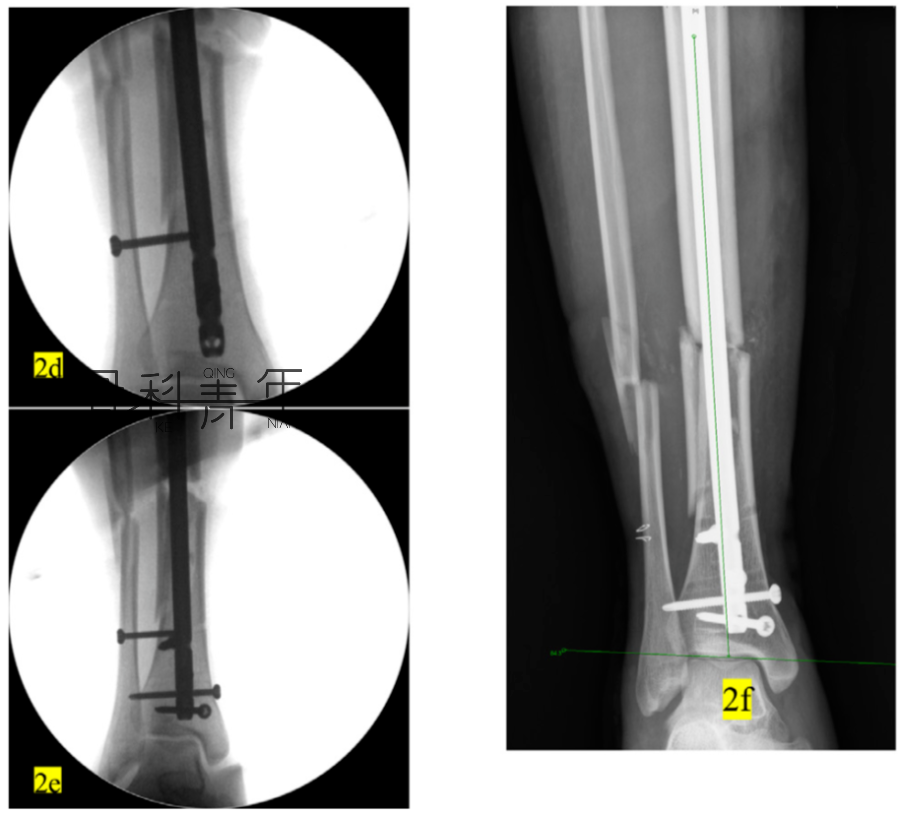
图 在人工智能辅助下骨折检测诊断性能的提高
总之,人工智能辅助提高了影像科医生和非影像科医生对涉及各种解剖位置的骨折检测的敏感性,甚至可提高特异性。该技术还减少阅读X线光片所需的时间。
原文出处:
Ali Guermazi,Chadi Tannoury,Andrew J Kompel,et al.Improving Radiographic Fracture Recognition Performance and Efficiency Using Artificial Intelligence.DOI:10.1148/radiol.210937
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#X线#
52
#X线片#
47
神奇!
71
学习了
72