European Radiology:钆基造影剂对多发性硬化症患者脑萎缩自动测量的影响
2022-04-15 shaosai MedSci原创
在过去三十年里,GBCA的使用不断增加。然而,这些数据对脑萎缩测量的价值取决于我们在自动图像分析中正确解释这些数据的能力。
 研究显示,多发性硬化症(MS)患者在MRI上测量的灰质(GM)萎缩反映了中枢神经系统不可逆的神经轴突损失和神经退行性改变。GM萎缩的程度与身体和认知障碍持续相关,是一个有临床前景的神经退行性生物标志物。此外,随着对神经保护性干预的需求增加,GM萎缩是一种容易获得的结果测量方法。
研究显示,多发性硬化症(MS)患者在MRI上测量的灰质(GM)萎缩反映了中枢神经系统不可逆的神经轴突损失和神经退行性改变。GM萎缩的程度与身体和认知障碍持续相关,是一个有临床前景的神经退行性生物标志物。此外,随着对神经保护性干预的需求增加,GM萎缩是一种容易获得的结果测量方法。
目前有许多可用的方法和软件来测量GM萎缩。虽然FreeSurfer需要大量的处理时间,虽然不太适合临床实践,但它是研究中最常用的自动化方法之一。在关于多发性硬化症的GM萎缩的文献中,许多重要的论文都使用了FreeSurfer。
由于非增强的三维(3D)T1加权图像具有较高的组织对比度,因此脑部分割软件常使用该序列图像进行评估。然而,非增强的三维T1加权图像在多发性硬化症标准脑MRI方案中并不是强制性的,因此不会被常规纳入。相反,强化后的T1加权图像往往是优先考虑的序列之一。在持续炎症的情况下,静脉注射的造影剂会在血脑屏障(BBB)被破坏的地方渗入脑实质,可以明确地发现有活动性炎症的病灶。
在过去三十年里,GBCA的使用不断增加。然而,这些数据对脑萎缩测量的价值取决于我们在自动图像分析中正确解释这些数据的能力。GBCA对萎缩测量的影响在很大程度上仍是未知的。
近日,发表在European Radiology杂志的一项研究验证了使用GBCA增强后的T1加权图像进行体积和皮质厚度测量,并就如何解释临床上相关的和普遍考虑的测量结果提供了指导。
本研究共纳入了22名多发性硬化症患者,使用同一扫描仪进行检查,以相同的采集方案获得使用钆基造影剂(GBCA)之前和之后的三维T1加权MR图像。使用两个FreeSurfer版本(v.6.0.1和v.7.1.1.)来计算灰质(GM)和白质(WM)体积以及全脑和区域皮质厚度。通过类内相关系数(ICC)评估强化前和强化后图像所获得的测量结果之间的一致性,通过配对t检验调查差异,并计算WM和GM物质总体积、深层GM和丘脑总体积以及平均皮质厚度的平均增加或减少百分比。
所有调查指标之间都有良好到优秀的可靠性,ICC从0.926到0.996不等,所有P值都<0.001。在对比后的图像中,GM体积和皮质厚度测量值明显增加了3.1-17.4%,而WM总体积明显减少了1.7%(所有P值均<0.001)。
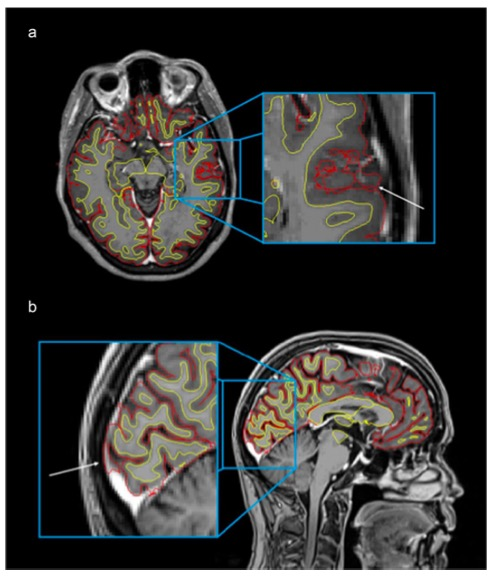
图 强化T1加权MRI,显示WM和GM之间的边界(白色表面)(黄色),以及GM和CSF之间的边界(皮层表面)(红色)
本研究表明,FreeSurfer可以从强化后的三维T1加权图像中获得可靠的GM萎缩测量结果。从GBCA给药前后获得的图像中得到的所有调查的GM和WM测量值之间都有很好到很好的一致性。然而,由于强化后图像中GM的系统性高估,从强化前后图像中获得的测量结果不应直接进行比较,而且从某些区域(如颞部)提取的测量结果应谨慎应用。此外,应研究可能的系统性影响,这些影响取决于GBCA的剂量和注射后的延迟时间,这为后续的研究提供了参考。
原文出处:
Ingrid Anne Lie,Emma Kerklingh,Kristin Wesnes,et al.The effect of gadolinium-based contrast-agents on automated brain atrophy measurements by FreeSurfer in patients with multiple sclerosis.DOI:10.1007/s00330-021-08405-8
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#钆基造影剂#
54
#自动测量#
69
#PE#
39
#多发性#
47
#萎缩#
0
#硬化症#
35
#脑萎缩#
27
#造影#
29