ACC 2020:阿司匹林与房颤患者30天出血量增加\缺血风险降低相关(AUGUSTUS研究)
2020-04-06 MedSci MedSci原创
对于房颤合并急性冠脉综合征(ACS)或者接受了经皮冠状动脉介入治疗(PCI)的患者,其抗栓治疗存在挑战,三联还是双联治疗一直存在争议。
对于房颤合并急性冠脉综合征(ACS)或者接受了经皮冠状动脉介入治疗(PCI)的患者,其抗栓治疗存在挑战,三联还是双联治疗一直存在争议。
根据3月29日在ACC.20 / WCC上进行的特色临床研究会议期间发表的AUGUSTUS试验的事后分析结果,该结果同时在《循环》杂志上发表。在最近患有急性冠状动脉综合征(ACS)和/或PCI且服用apixaban或维生素K拮抗剂的房颤(AFib)患者中,服用阿司匹林可能会导致出血风险增加和缺血风险降低之间长达30天的等量平衡。
2019年ACC会议上公布结果显示,对于近期发生ACS或接受PCI的房颤患者,阿哌沙班+P2Y12抑制剂的双联抗栓治疗方案与华法林+双联抗血小板的三联治疗方案相比,出血风险显著降低,缺血事件发生率无显著差异。新型口服抗凝药(NOAC)+P2Y12抑制剂的联合方案可以显著降低出血风险而且不增加血栓事件。
在这项回顾性研究中,John H. Alexander博士等人设计了三个复合性出血结局和三个复合性缺血结局,以观察阿司匹林与安慰剂的风险-收益权衡,以及apixaban或VKA在30天和6个月时的效果。最初的AUGUSTUS试验表明,安慰剂组与新近ACS和/或PCI并接受P2Y12抑制剂和apixaban或VKA的AFib患者相比,阿司匹林的出血更少。
AUGUSTUS试验是一项国际、随机、双盲、安慰剂对照试验,采用2 x 2因子设计,评估了双联抗栓治疗(不用阿司匹林)对出血风险高且同时存在心梗、卒中和血栓风险人群的有效性和安全性。
该试验在33个国家纳入了4,614名患者,包括美国、加拿大、墨西哥、英国以及其他欧洲、亚洲和南美洲国家。患者的中位年龄为70岁,男性占71%。患者均有房颤,需要长期(超过6个月)接受抗凝治疗,而且近期发生过ACS和/或置入支架,均存在抗血小板治疗的适应证。超过92%的患者在基线时服用氯吡格雷,其他患者服用了普拉格雷或者替格瑞洛。该试验招募了4,614名中位年龄为71岁的患者,所有患者均具有出血和缺血性事件的高风险。适应症为ACS合并PCI的患者占37%,药物治疗的ACS患者占24%,择期PCI的患者占39%。
在ACS发病或者置入支架后14天内,患者接受两次随机分配:首先,随机分配到阿哌沙班组或者华法林组;然后,随机分配到阿司匹林组或者安慰剂组(双盲)。所有患者均治疗6个月。选择这一随访时间是因为大多数出血事件、心梗、卒中和血栓形成都发生在ACS发病或置入支架后前6个月。

图1 研究设计
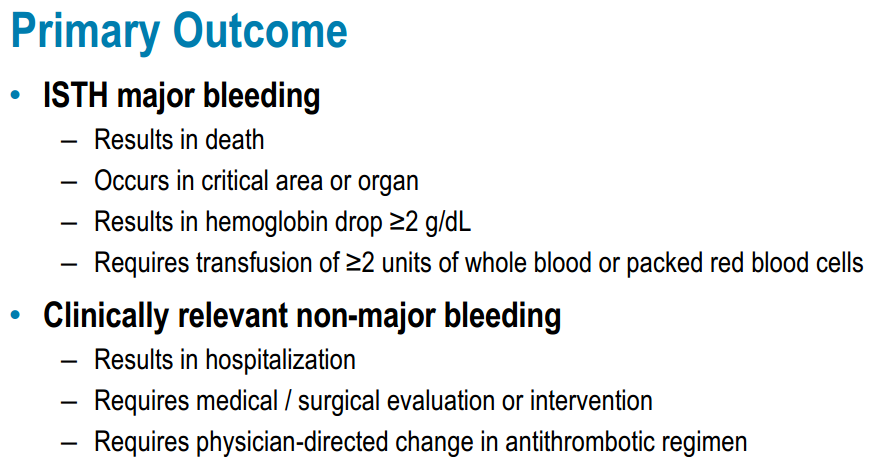
图2 主要终点定义
根据结果,30天内阿司匹林最多可增加严重出血量,并减少缺血事件。在30天时,服用阿司匹林的患者发生复合性出血的绝对风险范围从严重出血的2.1%到广泛出血的7.5%(致命、颅内、ISTH严重、出血住院、临床相关的非重大出血),而服用安慰剂的严重出血为1.1%,患者大出血率为4.0%。在服用阿司匹林的患者中,缺血性复合结果的绝对风险范围从重度事件的1.7%至广泛事件的6.7%,而安慰剂组中重度事件的2.6%至广泛事件的6.8%。
研究表明,30天后,这种平衡没有持续。对于出血结局,阿司匹林组的绝对风险范围为严重出血的3.7%至广泛出血的12.1%,而安慰剂组的严重出血为2.5%,广泛出血为7.2%。在服用阿司匹林的患者中,缺血性事件的绝对风险范围从严重事件的3.8%到广泛事件的14.3%,而在安慰剂组中,严重事件为4.0%,广泛事件为14.3%。
研究人员说,除了P2Y12抑制剂或口服抗凝剂外,使用阿司匹林长达30天还可以在增加出血风险和降低缺血性事件风险之间取得平衡。30天后,阿司匹林可导致出血增加,而不会减少缺血事件。他们的结论是,这些发现有助于为经历过ACS和/或PCI的AFib患者提供有关抗栓治疗的循证决策,并有助于以患者为中心的共同决策。
2019年报告相关结果如下:
主要安全性终点结果显示,与服用华法林的患者相比,阿哌沙班治疗患者的风险降低了31%(10.5% vs 14.7%;HR, 0.69; 95%CI, 0.58 to 0.81; P<0.001 非劣效性和优效性);与服用阿司匹林的患者相比,安慰剂组风险降低了47%(16.1% vs 9.0%;HR, 1.89; 95% CI, 1.59 to 2.24; P<0.001)。
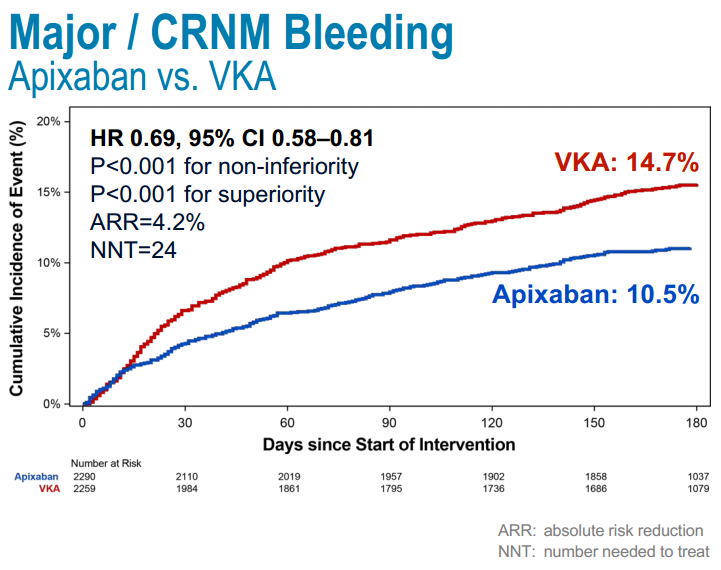
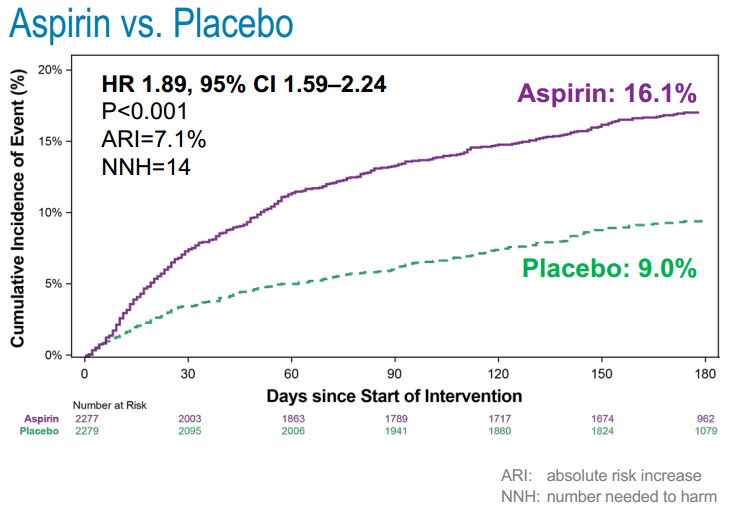
图3 主要终点
氯吡格雷+华法林+阿司匹林治疗组患者出血事件发生率最高(18.5%),氯吡格雷+阿哌沙班+安慰剂治疗组发生率最低(7.3%)。
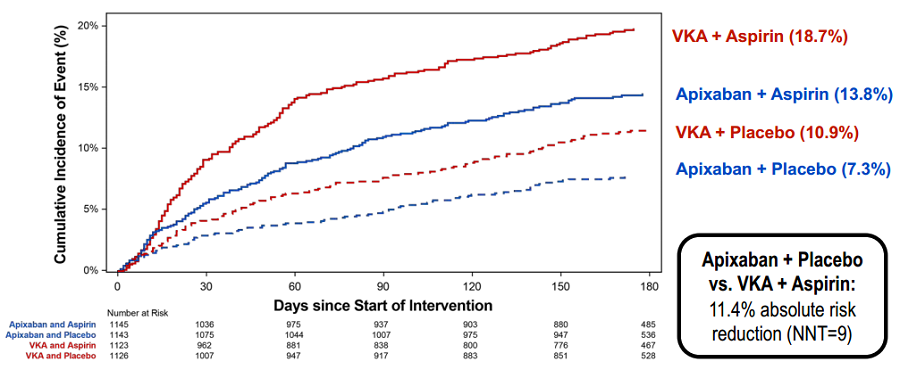
图4 主要终点在四组患者中的比较
阿哌沙班组的死亡或住院比例低于华法林组(23.5% vs. 27.4%; HR, 0.83; 95% CI, 0.74 to 0.93; P=0.002);阿司匹林组的死亡或住院比例与安慰剂组相似。
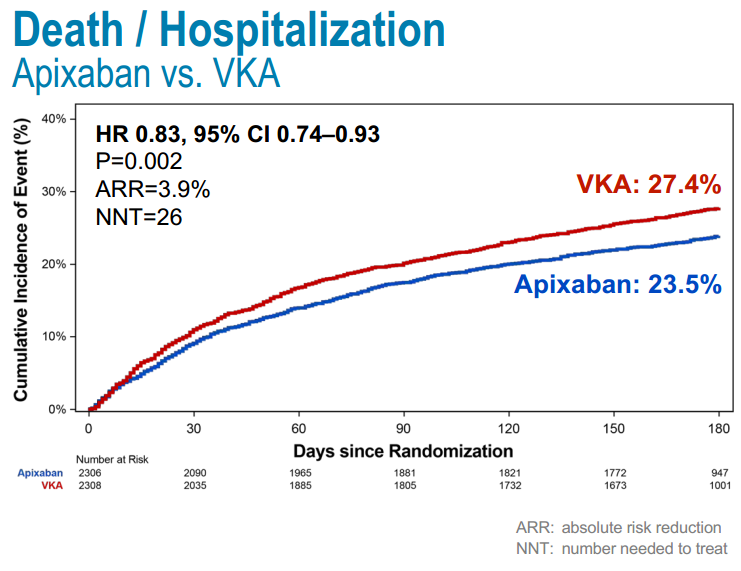
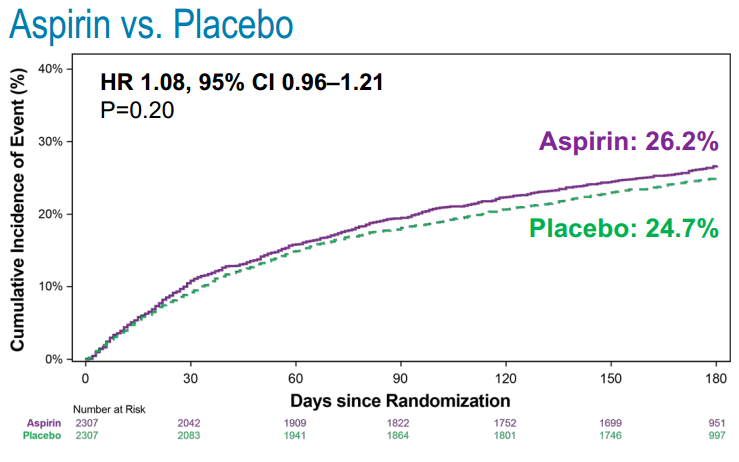
图5 死亡/住院复合终点的比较
氯吡格雷+华法林+阿司匹林治疗组患者的死亡或住院比例最高(27.5%),氯吡格雷+阿哌沙班+安慰剂治疗组比例最低(22.0%)。
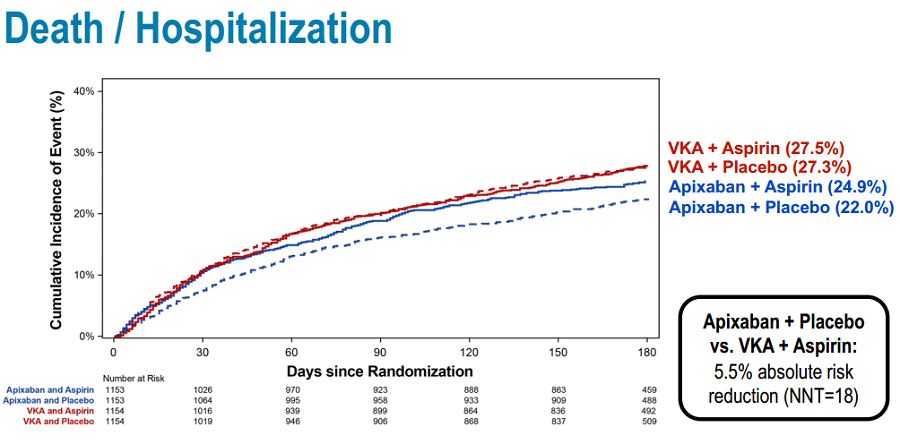
图6 死亡/住院复合终点在四组患者中的比较
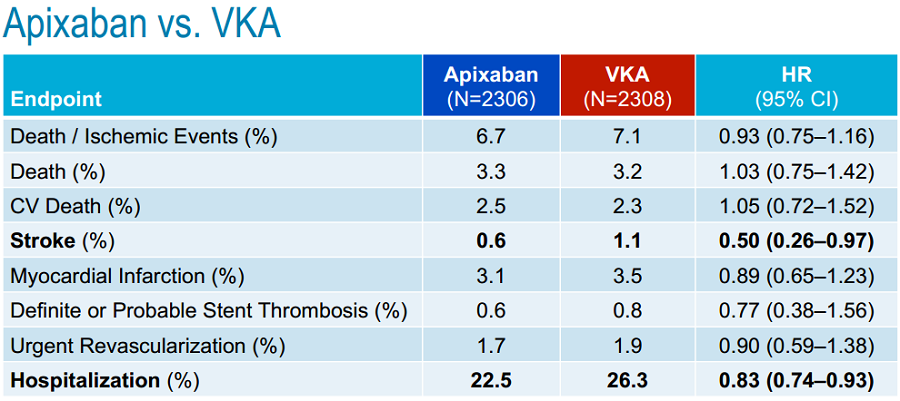
阿哌沙班组与华法林组的缺血事件发生率相似;与华法林相比,阿哌沙班治疗患者的卒中风险降低了50%。阿司匹林组的缺血事件发生率与安慰剂组相似。
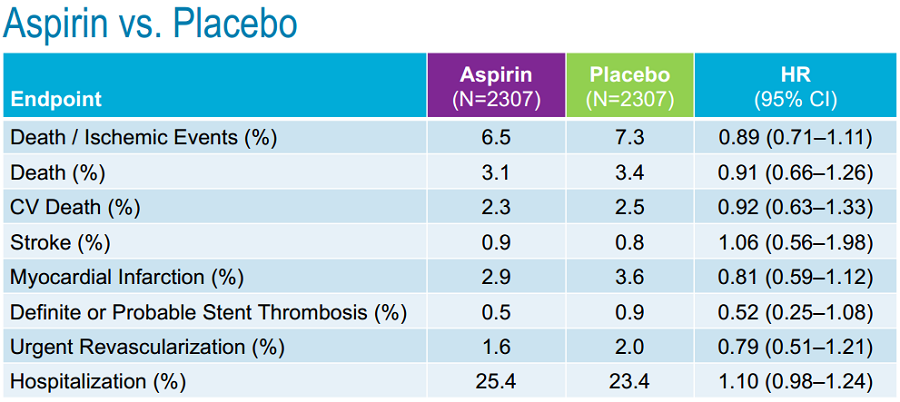
表1 缺血终点的比较
原始出处:
Alexander JH, Wojdyla D, Vora AN, Thomas L, Granger CB, Goodman SG, Aronson R, Windecker S, Mehran R, Lopes RD.The Risk / Benefit Tradeoff of Antithrombotic Therapy in Patients with Atrial Fibrillation Early and Late After an Acute Coronary Syndrome or Percutaneous Coronary Intervention: Insights from AUGUSTUS.Circulation. 2020 Mar 29. doi: 10.1161/CIRCULATIONAHA.120.046534.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#风险降低#
40
不错
82
#ACC 2020#
68
#30天#
42
#出血量#
41
#ACC#
41
#房颤患者#
44
房颤,临床上碰到很多哦
70