Neurology:后循环卒中后双侧肥大性橄榄核变性
2017-11-21 杨中华 脑血管病及重症文献导读
肥大性橄榄核变性是一种跨突触变性,累及相互联系的下橄榄核、红核和对侧齿状核(Guillain-Mollaret三角)纤维。橄榄核对称性肥大和T2高信号有助于和脱髓鞘、肿瘤和炎症鉴别。
40岁,男性。
4个月前后循环卒中,来院就诊。
查体,昏迷,四肢痉挛,双侧跖伸肌反射阳性,软腭痉挛。
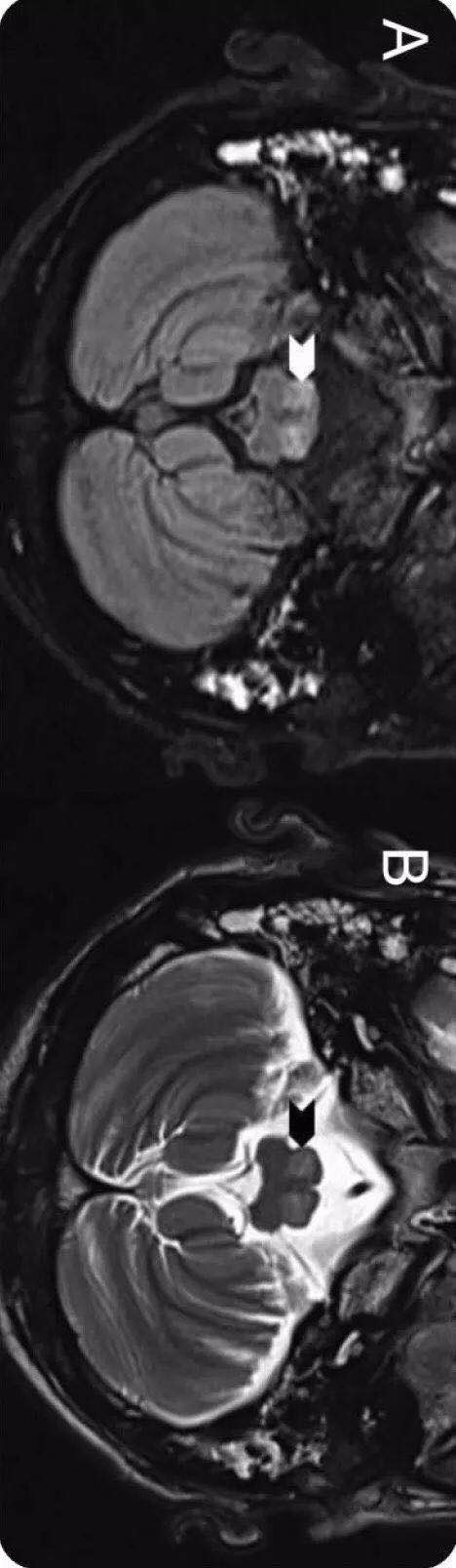
头MRI显示橄榄核肥大(下图),图A为Flair图B为T2显示延髓橄榄核肥大和高信号(白和黑箭头):
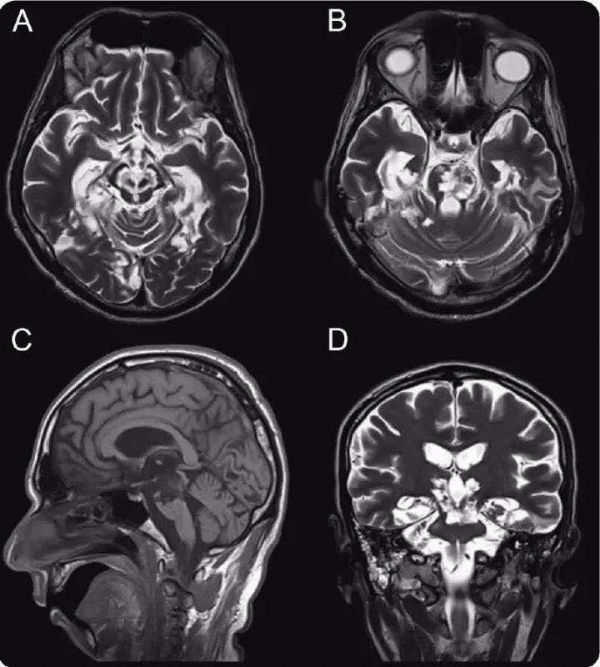
头MRI还发现中脑和桥脑慢性梗死(下图),提示脑梗死4个月后出现肥大性橄榄核变性。图A和B为轴位T2,图C为矢状位T1,图D为冠状位T2,显示中脑、桥脑、右侧小脑半球和双侧颞叶内侧面慢性梗死:
肥大性橄榄核变性是一种跨突触变性,累及相互联系的下橄榄核、红核和对侧齿状核(Guillain-Mollaret三角)纤维。橄榄核对称性肥大和T2高信号有助于和脱髓鞘、肿瘤和炎症鉴别。
原始出处:
Manchikanti Venkatesh, et al. Teaching NeuroImages: Bilateral hypertrophic olivary degeneration following posterior circulation stroke. Neurology. 2017 Oct 31
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#肥大性#
38
#卒中后#
22
#后循环卒中#
43
#Neurol#
35
#变性#
23
#双侧#
31