Nature Medicine:许韧博士等报道靶向骨特异性血管的促成骨化新机制——邹卫国、罗剑点评
2018-05-24 迦 溆 BioArt
随着全球老年化的加剧,骨质疏松骨折患者逐年递增,被世界卫生组织(WHO)称为“无声无息的流行病”。尤其在女性更年期后,高龄骨折直接或间接的致死率已与乳腺癌持平。健康成人体内,成骨细胞介导的骨形成与破骨细胞介导的骨吸收维持着正常的骨代谢稳态,其中骨形成减少和骨吸收增多均可以导致骨质疏松等常见代谢类疾病。然而目前用于治疗骨质疏松的药物大多集中在抑制破骨细胞的功能和分化上,并不能直接作用于成骨细胞。
随着全球老年化的加剧,骨质疏松骨折患者逐年递增,被世界卫生组织(WHO)称为“无声无息的流行病”。尤其在女性更年期后,高龄骨折直接或间接的致死率已与乳腺癌持平。健康成人体内,成骨细胞介导的骨形成与破骨细胞介导的骨吸收维持着正常的骨代谢稳态,其中骨形成减少和骨吸收增多均可以导致骨质疏松等常见代谢类疾病。然而目前用于治疗骨质疏松的药物大多集中在抑制破骨细胞的功能和分化上,并不能直接作用于成骨细胞。
俗话说“旧的不去,新的不来”,一味抑制骨吸收并不能直接促进体内新生骨的形成反而会引起药物相关的副作用。此外,临床上唯一的可以高效促进骨形成的药物-甲状旁腺激素还存在着两年使用时限和骨折治疗不敏感等弊端。所以,当前骨形成药物的开发“瓶颈”急需新的策略和机制来解决。
在代谢过程中,器官和组织不同的结构性和代谢需求促进了特异性血管的形成,这些特异性的血管会传递引导组织向其目标发育的分子。这种进程需要器官和血管之间的信号协同作用:器官产生能够吸引血管朝向代谢活跃区域发展的局域性生长因子,而血管会释放对于发育中器官细胞分化有影响的分子。骨稳态代谢也不例外,这种组织特异性的血管亚型-骨H型(CD31hiEMCNhi)血管(图一)于2014年由Ralf Adams组在Nature以背靠背论文的形式发表揭示,然而骨特异血管和骨形成的串扰机制及其在骨骼疾病治疗中的功能还有待进一步解明。
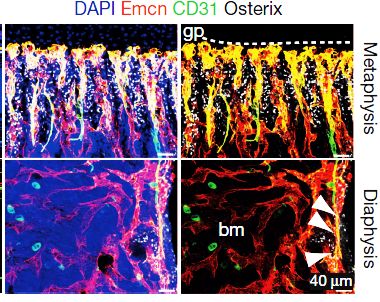
图一:组织特异性的血管亚型-骨H型(CD31hiEMCNhi)血管
在骨形成过程中,复杂基因网络调控着成骨细胞的分化、细胞外基质的形成、矿化等各个过程,以确保骨组织在力学、代谢等各方面中的生理功用。美国康奈尔大学的许韧博士一直聚焦于骨稳态的微环境研究,早在日本读博期间,就已以共同第一作者身份在Nature上发文,首次证明了骨腔内的感觉神经嵌入能够有效地调节成骨细胞活性及其介导的骨稳态。针对骨腔内神经和血管的分布并行性,许韧博士于博后阶段,将其在日本的骨神经研究延展到骨血管的层面,师从美国科学院院士Laurie H.Glimcher(前康奈尔大学医学院院长),并与病理学Matthew B. Greenblatt团队精诚协作,进一步拓展了对骨形成微环境的认识:发现了成骨细胞与骨血管内皮细胞之间的对话新机制,为骨代谢疾病的治疗和药物研发提供了新的思路和理论铺垫。该工作以“Targeting skeletal endothelium to ameliorate bone loss”为题以长文形式于5月21日发表在Nature Medicine上。
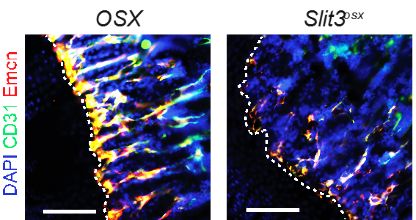
该研究团队首先以Schnurri-3 (SHN3)敲除所导致的高骨量小鼠为切入口,进一步发现该小鼠不仅仅表现为骨形成速率升高,同时表现为骨H型(CD31hiEMCNhi)血管的增加。通过RNA测序分析发现,在成骨细胞中,SHN3通过抑制ERK活性来负调控血管形成因子SLIT3的转录和表达,当SHN3敲除时,成骨细胞分泌更多的SLIT3,从而促进H型血管的形成。反之,在成骨细胞或骨细胞特异性基因敲除的小鼠模型中, SLIT3的缺失则可减少H型血管的形成(图二),进而导致骨形成速率的下降和骨质疏松表型的出现。有意思的是,进一步的基因和组织学分析表明H型血管本身并不生成SLIT3这一血管生成因子,而只大量表达其受体基因Robo1,证明了成骨来源SLIT3的重要性。Robo1基因敲除小鼠同样呈现H型血管的形成减弱和骨质疏松表型进一步验证了SLIT3/ROBO1通道在骨形成中的重要性。
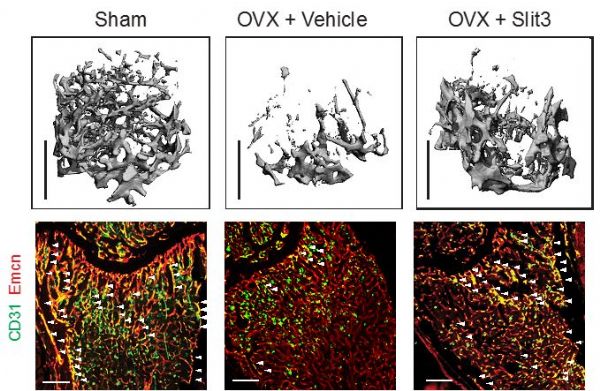
依据上述生理学的发现,研究者进一步深入分析了SLIT3介导的成骨细胞-内皮细胞对话在骨折愈合中的作用,发现敲除SLIT3延迟骨折愈合,而敲除SHN3可间接通过增加SLIT3的表达来促进骨折愈合。此外,在小鼠骨骼疾病模型中,给予局部或全身SLIT3重组蛋白时,可通过增加H型血管的形成来有效促进骨折愈合并缓解雌性更年期所导致的骨质疏松(图三)。
图三:SLIT3促进H型血管的形成
本研究工作的推进,揭示了成骨细胞与骨微环境中血管内皮细胞的相互对话的机制及其在骨再生和骨代谢平衡中的重要作用。
据悉,许韧博士为第一作者,Laurie H.Glimcher院士和Matthew B. Greenblatt博士为共同通讯作者。
原始出处:
Xu R, Yallowitz A, Qin A, et al.Targeting skeletal endothelium to ameliorate bone loss.Nat Med. 2018 May 21. doi: 10.1038/s41591-018-0020-z. [Epub ahead of print]
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CIN#
16
#特异性#
0
#Nat#
32
#DIC#
27
#成骨#
22
#Medicine#
20
#Med#
22
前沿研究.学习了.
66
学习
60