Clin Cancer Res:帕博西尼+氟维司群联合方案或可成为晚期乳腺癌的标准疗法
2022-06-24 MedSci原创 MedSci原创
帕博西尼+氟维司群联合方案或可成为HR+HER2-晚期乳腺癌的标准疗法。
帕博西尼(Palbociclib)是首批口服活性细胞周期蛋白依赖性激酶4/6(CDK4/6)抑制剂,已获批用于治疗激素受体阳性、人表皮生长因子受体2阴性(HR+HER2-)晚期乳腺癌(ABC)。3期PALOMA-3研究显示,帕博西尼联合氟维司群相比安慰剂联合氟维司群可显著延长HR+HER2-晚期乳腺癌患者的无进展生存期(11.2个月 vs 4.6个月,p<0.0001)。但中位随访了44.8个月时,帕博西尼组的总生存期虽长于安慰剂组(34.9个月 vs 28.0个月),但无显著性(p=0.0429)。
因此,研究人员延长了该试验的随访时间,以进一步分析两组的总生存期,同时评估循环肿瘤DNA(ctDNA)分子分析的预后价值。
在该试验中,HR+HER2-的晚期乳腺癌患者被随机(2:1)分成两组,分别接受帕博西尼(125mg/日,3/1周方案)+氟维司群(500mg)或安慰剂+氟维司群治疗。本次分析是在75%的入组患者死亡后进行的(393例死亡/521位患者)。
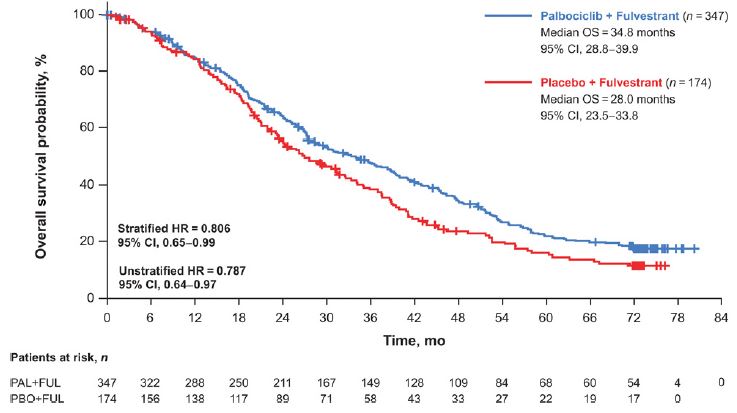
两组的总生存率
截止2020年8月17日,中位随访了73.3个月,帕博西尼组和安慰剂组分别发生了258例和135例死亡。帕博西尼组和安慰剂组的中位总生存期分别是34.8个月和28.0个月(分层风险比 0.81)。帕博西尼组和安慰剂组的六年总生存率分别是19.1%和12.9%。
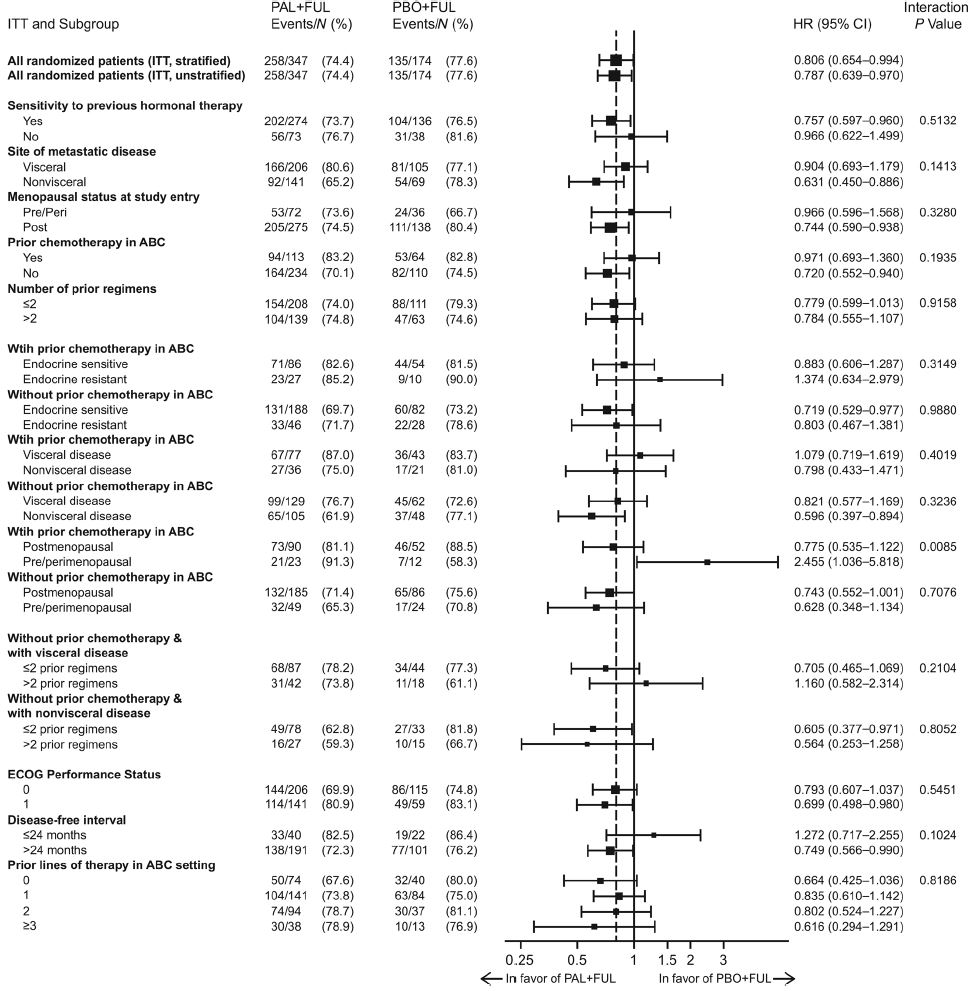
总生存率的亚组分析
此外,在大部分亚组中都观察到了帕博西尼+氟维司群治疗优于安慰剂+氟维司群的总生存期,特别是内分泌治疗敏感的患者、既往未接受过针对ABC化疗的患者和低循环肿瘤分数的患者,而且无论ESR1、PIK3CA或TP53基因的突变状态如何。最后,未观察到新的安全性问题。
总之,该研究延长随访的分析结果显示,帕博西尼联合氟维司群治疗可显著改善HR+HER2-晚期乳腺癌患者的生存期,而且维持时间长达6年之久,支持将该联合方案作为这类患者的标准疗法。
原始出处:
Massimo Cristofanilli, Hope S. Rugo, Seock-Ah Im, et al. Overall Survival with Palbociclib and Fulvestrant in Women with HR+/HER2- ABC: Updated Exploratory Analyses of PALOMA-3, a Double-blind, Phase III Randomized Study. Clin Cancer Res 2022; https://doi.org/10.1158/1078-0432.CCR-22-0305.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#联合方案#
51
#标准疗法#
54
#帕博西尼#
53