JACC:双链小干扰RNA Inclisiran可有效降低多种高胆固醇血症患者的低密度脂蛋白胆固醇!
2021-03-07 Nebula MedSci原创
第一个也是唯一使用小分子干扰RNA(siRNA机制)降低低密度脂蛋白胆固醇LDL-C的疗法
Inclisiran是一种双链小干扰RNA,能抑制肝脏中原蛋白转换酶枯草杆菌毒素-kexin 9型(PCSK9)的翻译,从而降低低密度脂蛋白胆固醇(LDL-C)和其他致动脉粥样硬化的脂蛋白,每年只需要用两次。
2020年10月,Inclisiran获得欧盟CHMP推荐,建议批准用于治疗原发性胆固醇血症(杂合子家族和非家族性)或混合型血脂异常成人患者。但还获得FDA批准。
本研究目的是对Inlisiran的3项3期研究(ORION-9、ORION-10和ORION-11)进行患者水平的综合分析。
ORION-9试验评估了Inclisiran治疗对杂合性家族性高胆固醇血症(HeFH)患者LDL-C的影响;ORION-10试验评估了Inclisiran用于动脉粥样硬化性心血管疾病(ASCVD)和高LDL-C的患者的疗效;ORION-11试验评估了Inlisiran用于ASCVD和ASCVD风险相等的患者的疗效;所有患者均采用最大耐受剂量他汀药物±其他降LDL-C药物作基础治疗。
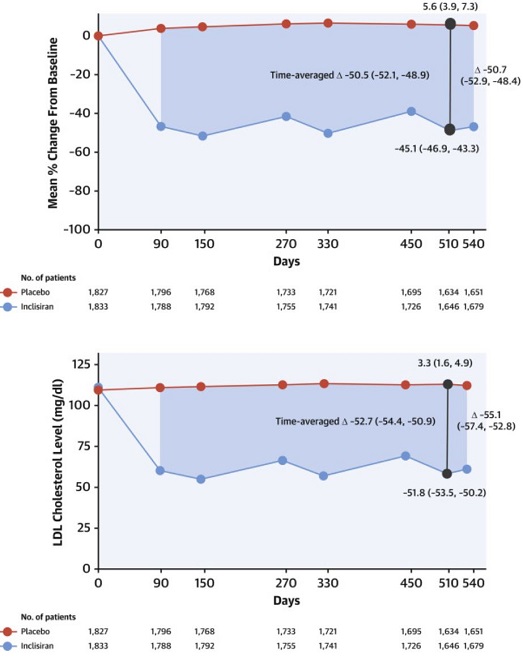
受试患者按1:1随机分组接受Inlisiran或安慰剂,在第1天和第90天以及随后每间隔6个月皮下注射一次,共540天。共同的终点是LDL-C的百分比变化。
LDL-C的变化
共纳入3660名患者。第510天时,Inlisiran组患者的LDL-C经安慰剂校正后的变化为-50.7%(95%CI:-52.9%~-48.4%;P<0.0001)。相应的按时间校正后的LDL-C的变化为-50.5%(95%CI:-52.1%~-48.9%;P<0.0001)。两组的安全性相似。Inlisiran组的注射部位的紧急治疗不良事件多于安慰剂组(5.0% vs 0.7%),但主要是轻微的,没有严重或持续性的。两组间的肝肾功能测试、肌酸激酶值和血小板计数没有显著差异。
综上,该汇总分析显示,在最大耐受剂量他汀药物±其他降LDL-C药物治疗的基础上,Inlisiran,每年用两次,可以降低杂合性家族性高胆固醇血症、ASCVD或ASCVD风险相同的成年患者的LDL-C,是一种有效、安全且耐受性良好的治疗方法。
原始出处:
Wright R Scott,Ray Kausik K,Raal Frederick J et al. Pooled Patient-Level Analysis of Inclisiran Trials in Patients With Familial Hypercholesterolemia or Atherosclerosis. J Am Coll Cardiol, 2021, 77: 1182-1193.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JACC#
34
#ACC#
36
#高胆固醇血症#
38
#脂蛋白#
42
。
81
希望能尽快用于临床。
82