Diabetes Care:1型糖尿病、MODY2和健康对照组儿童肠道菌群的组成和功能存在差异
2021-09-01 MedSci原创 MedSci原创
肠道菌群及其相关代谢产物在血糖代谢、胰岛素抵抗以及慢性炎症等2型糖尿病的病理和生理中发挥着重要的作用。
糖尿病属是由于胰岛素分泌绝对或相对不足,导致血糖的代谢和利用产生紊乱。有研究表明,肠道菌群结构和功能上的变化与高血糖、胰岛素抵抗有很大的关系,也就是说,肠道菌群及其相关代谢产物在血糖代谢、胰岛素抵抗以及慢性炎症等2型糖尿病的病理和生理中发挥着重要的作用。
近年来,科学家们通过研究阐明了糖尿病和机体肠道之间的关联,研究者表示,肠道微生物组的改变或能帮助预测和监测机体疾病的进展。
本文就来谈谈糖尿病与肠道菌群的关系。
目的:1型糖尿病与肠道菌群组成差异有关。到目前为止,还没有对青年人中成年发病型糖尿病(MODY2)进行微生物研究,MODY2是单基因遗传突变的糖尿病类型。比较了1型糖尿病、MODY2和健康对照组的肠道菌群。
研究设计与方法:这是一项病例对照研究,对象为15名1型糖尿病儿童、15名MODY2儿童和13名健康儿童。代谢和影响肠道菌群的潜在因素得到控制。16S rRNA焦磷酸测序测定微生物的组成。
结果:与健康对照组相比,1型糖尿病患者菌群多样性显著降低,类杆菌、反刍球菌、韦龙氏菌、布鲁氏菌和链球菌属的相对丰度显著升高,双歧杆菌、玫瑰百合菌、粪便杆菌和泪腺螺旋菌的相对丰度显著降低。MODY2的普氏杆菌丰度较高,反刍球菌和类杆菌丰度较低。促炎细胞因子和脂多糖在1型糖尿病患者中增加,肠道通透性(由带状蛋白水平决定)在1型糖尿病患者和MODY2患者中显著增加。PICRUST分析发现,在1型糖尿病中,与脂质和氨基酸代谢、ABC转运、脂多糖生物合成、花生四烯酸代谢、抗原处理和呈递以及趋化因子信号通路相关的基因增加。
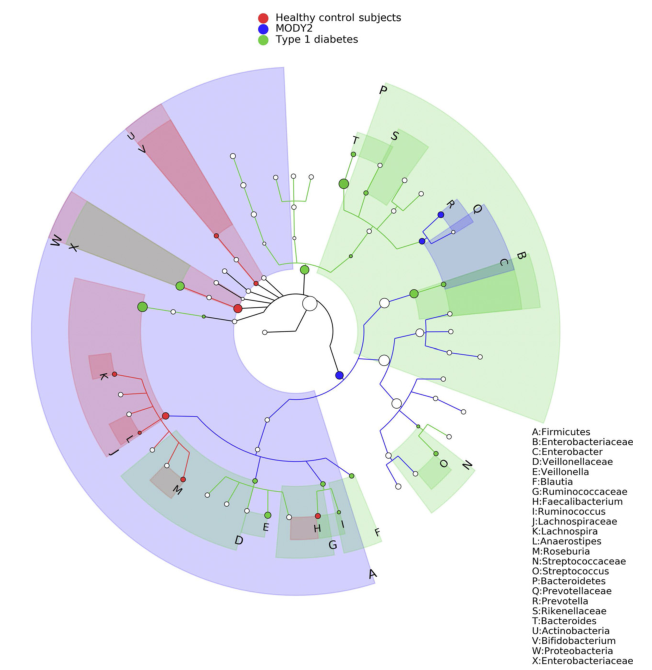
图 分支图显示了1型糖尿病、MODY2和健康对照组粪便微生物菌群的不同丰度的分类群。采用线性检验进行判别分析和效应大小分析
(Kruskal-Wallis检验,P=0.05),验证各研究组分类单元丰度差异的统计意义和效应大小。每个圆圈的直径与其丰度成正比。
结论:1型糖尿病患者肠道菌群不仅在分类学和功能水平上与健康受试者不同,而且在非自身免疫性糖尿病模型方面也存在根本差异。未来的纵向研究可以评估1型糖尿病高危患者肠道菌群的调节是否可以改变这种自身免疫性疾病的自然病史。
原文出处:
Leiva-Gea I, Sánchez-Alcoholado L, Martín-Tejedor B, et al. Gut Microbiota Differs in Composition and Functionality Between Children With Type 1 Diabetes and MODY2 and Healthy Control Subjects: A Case-Control Study. Diabetes Care. 2018. 41(11): 2385-2395.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#对照#
48
#BET#
44
#DIA#
37
#Diabetes#
54
#对照组#
39
#MODY#
42
#肠道菌#
39
谢谢MedSci提供最新的资讯
63