Front Oncol:可切除胰腺癌伴有淋巴结转移或R1切除使用辅助化疗续贯放化疗的疗效评估
2021-09-24 yd2015 MedSci原创
研究表明,对于可切除胰腺癌伴有淋巴结转移或R1切除患者,术后辅助化疗续贯放化疗(CT-CRT)可改善患者OS,值得进一步探讨。
胰腺癌的预后很差,5年生存率只有10-25%。可切除胰腺癌建议术后辅助化疗(CT),可改善预后,但是伴有淋巴结转移或R1切除患者的复发几率较高,并且跟较差的OS相关。目前研究表明辅助放疗并不能改善患者预后。初始研究发现辅助的放化疗(CRT)也不能改善预后,但是对于选择性的人群,比如伴有淋巴结转移或R1切除的患者,可以从CRT治疗中获益。因此,ASCO建议对于有淋巴结转移或R1切除的胰腺癌患者进行辅助化疗后可进行辅助放化疗。但是ESMO并没有推荐CRT治疗。对此,来自我国北京协和医院的团队开展了相关研究,相关结果发表在Frontiers in Oncology杂志上。
研究纳入266例可切除胰腺癌患者,伴有淋巴结转移或R1切除。148例(55.6%)为男性。69.2%的患者肿瘤位于胰头。91例患者接受了R1切除术。大多数患者肿瘤为T2期,TNM为II期。在淋巴结状态方面,少数患者(7.5%)无淋巴结转移,其中N1期63.9%,N2期28.6%。9.4%的患者接受了氟尿嘧啶为基础的CRT。
肿瘤位于胰腺头部的患者中位OS为19.0个月(95%Cl:15.8-22.2),而肿瘤位于胰腺体或尾部的患者中位OS为29.0个月(95%Cl:15.8- 42.2)(p=0.007)。接受GEM单药、吉西他滨+S-1(GS)和S-1单药治疗的患者中位OS分别为28.0个月(95% Cl: 19.2-36.8)、25.0个月(95% Cl: 16.2-33.8)和23.0个月(95% Cl: 12.1-33.9)(p<0.001)。T1期肿瘤患者的中位OS为37.0个月,T2和T3患者的中位OS均为20个月(p=0.008)。
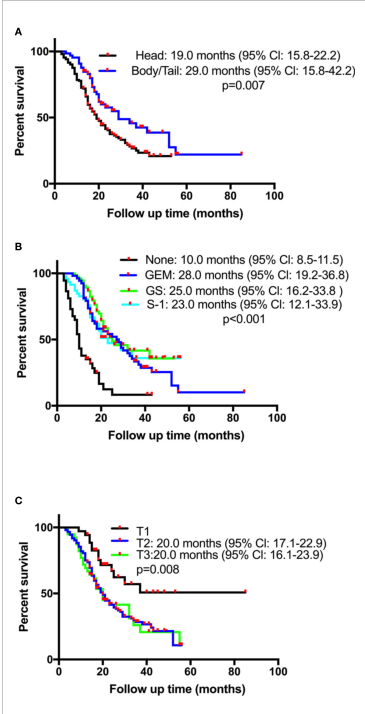
OS对比
在多变量Cox回归分析,胰腺体或尾部肿瘤(HR=0.433, p<0.0001,与胰头相比较),辅助CT-CRT (HR=0.369, p=0.015, 与单独辅助CT比较)和CT (GEM: HR=0.356, p<0.0001; GS: HR=0.269, p<0.0001; S-1: HR=0.325, p<0.0001, 与无化疗相比较)是较好的OS独立预测因素。肿瘤T分期越高,预后越差 (I期:参考; II期:HR=2.199, p=0.013; III期: HR=3.796, p<0.0001)。

OS相关因素分析
对122例患者进行倾向评分匹配,探讨CRT的作用。51例患者(CT组和CT-CRT组分别为31例和20例)通过匹配生成队列。进一步分析显示,与单纯CT相比,辅助CT-CRT可延长生存期(CT组和CT-CRT组中位OS分别为28个月和52个月,p=0.009),并且降低局部复发率(CT组和CT-CRT组分别为56.5%和21.4%)。
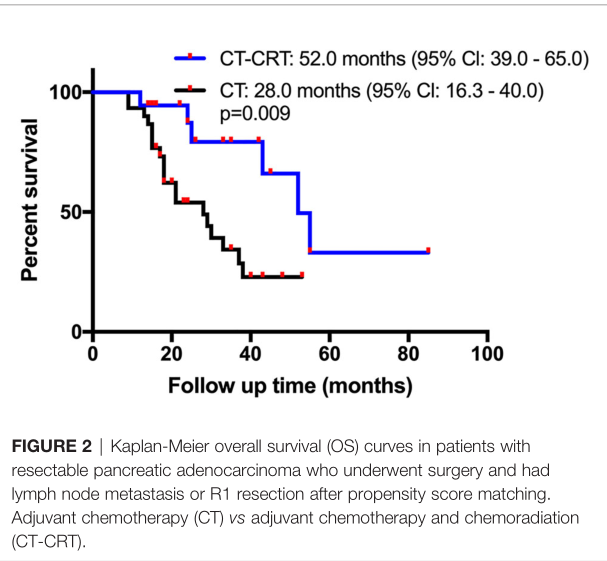
PSM比较OS
综上,研究表明,对于可切除胰腺癌伴有淋巴结转移或R1切除患者,术后辅助化疗续贯放化疗(CT-CRT)可改善患者OS,值得进一步探讨。
原始出处:
Xing J, Yang B, Hou X, et al. (2021) Prognostic Factors and Effect of Adjuvant Chemoradiation Following Chemotherapy in Resected Pancreatic Cancer Patients With Lymph Node Metastasis or R1 Resection. Front. Oncol. 11:660215. doi: 10.3389/fonc.2021.660215.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#疗效评估#
46
#Oncol#
36
签到
0
厉害
52
#放化疗#
32
#淋巴结#
27
#淋巴结转移#
32
研究表明,对于可切除胰腺癌伴有淋巴结转移或R1切除患者,术后辅助化疗续贯放化疗(CT-CRT)可改善患者OS,值得进一步探讨。
73