Clin Cancer Res:Durvalumab+Tremelimumab+放疗用于错配修复正常的转移性结直肠癌的疗效
2021-02-04 Nebula MedSci原创
在错配修复熟练(MMR-P)的转移性结直肠癌(mCRC)中,单用免疫检查点抑制剂(ICI)并不能获得预期疗效,单用放疗(RT)也不能带来客观的全身益处,两者联用是否会带来不一样的结局呢?
在错配修复熟练(MMR-P)的转移性结直肠癌(mCRC)中,单用免疫检查点抑制剂(ICI)并不能获得预期疗效,单用放疗(RT)也不能带来客观的全身益处。然而,在临床前和临床模型中,RT和ICI联合应用可以诱导系统性的抗肿瘤免疫。
在这项单中心的II期研究中,招募了化疗难治性的MMR-P mCRC患者,予以durvalumab(1500mg)+tremelimumab(75mg)治疗,每4周一次,外加RT。主要终点是非放射病灶的客观反应率(ORR)。治疗和疗效与外周免疫细胞谱相关。
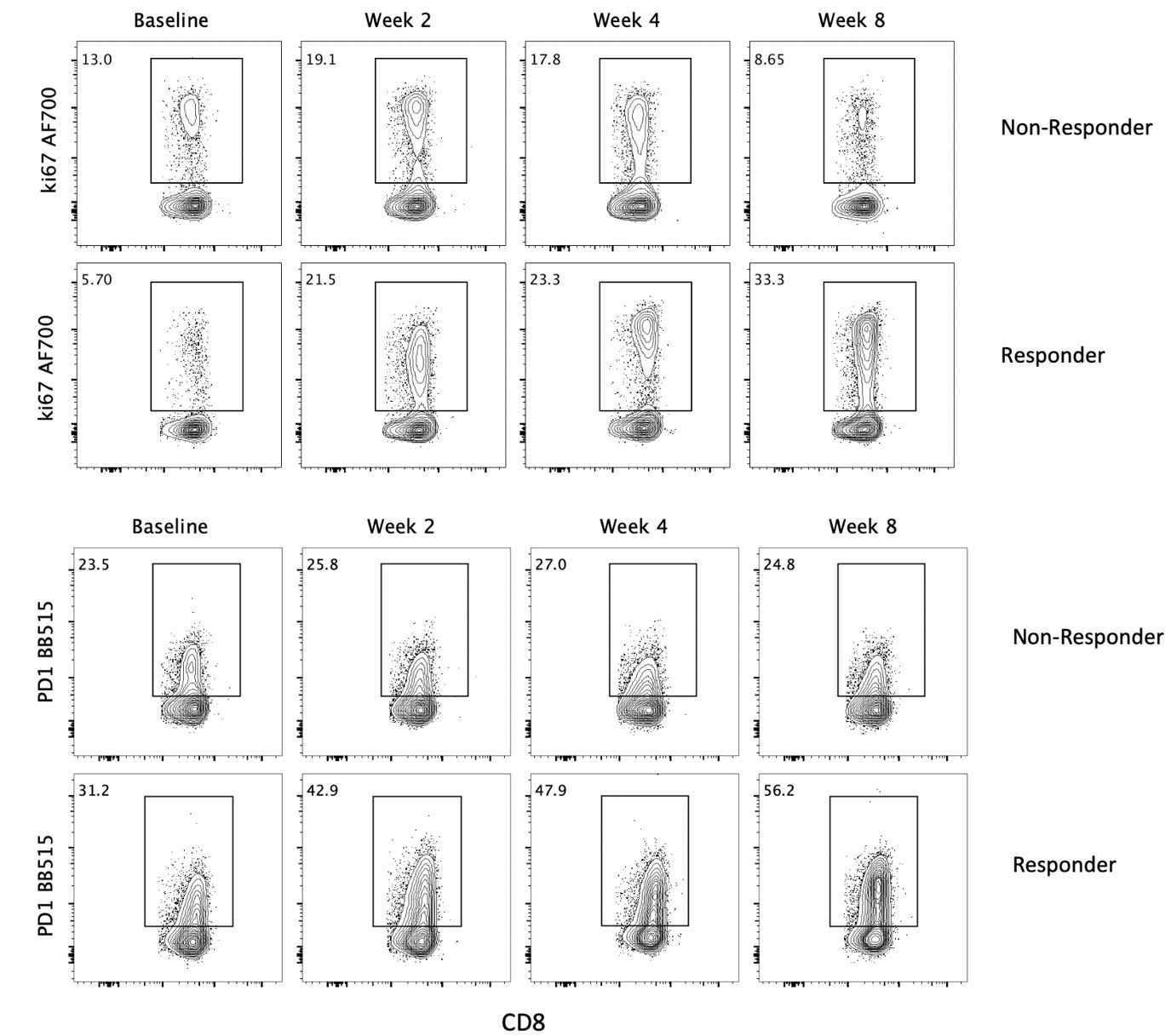
共招募了24名患者,中位随访时间为21.8个月(范围:15.9-26.3个月)。ORR为8.3%(2/24)(95%CI 1.0%~27.0%)。中位无进展生存期为1.8个月(95%CI 1.7~1.9个月),中位总生存期为11.4个月(95%CI 10.1~17.4个月)。25%的患者(n=6)出现了与治疗相关的3-4级不良事件。此外,研究人员观察到有客观反应的患者循环血液中CD8+T淋巴细胞活化、分化和增殖均有所增加。
总而言之,本研究评估的ICI+RT联合方案未达到预先指定的主要终点。然而,研究人员在非放射病灶中观察到了罕见的系统性免疫增强和消退(一种异常反应)。Durvalumab和tremlimumab+RT联合治疗MMR-P mCRC患者是可行的,且安全性可控。有必要对新免疫治疗联合方案进行进一步研究,并鉴定可预测异常反应的生物标志物。
原始出处:
Segal Neil H,Cercek Andrea,Ku Geoffrey Y et al. Phase II Single Arm Study of Durvalumab and Tremelimumab with Concurrent Radiotherapy in Patients with Mismatch Repair Proficient Metastatic Colorectal Cancer. Clin Cancer Res, 2021, https://doi.org/10.1158/1078-0432.CCR-20-2474
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#TREM#
41
#mAb#
36
#REM#
50
#Tremelimumab#
50
#转移性#
35
#结直肠#
42
谢谢梅斯提供这么好的信息,学到很多
53
每天进来学习了
83