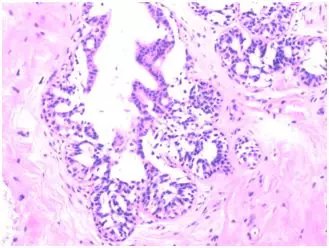
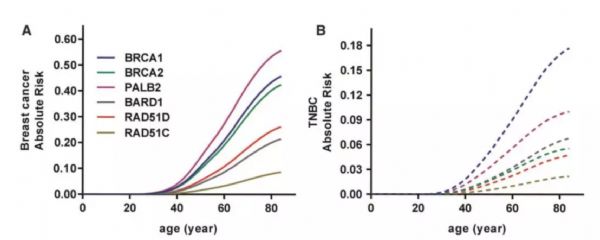
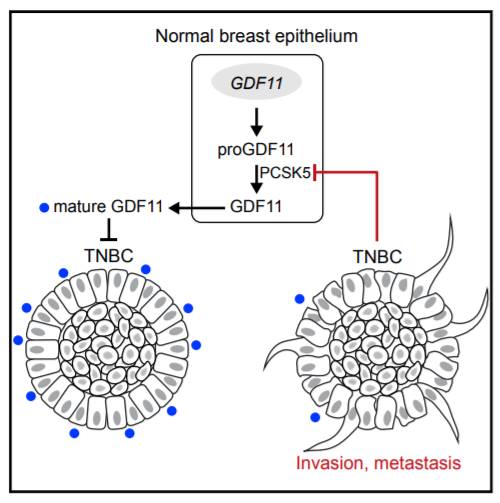
百例挑一:三阴性局部进展期乳腺癌新辅助化疗1例
2019-01-09 SHY 中国医学论坛报今日肿瘤
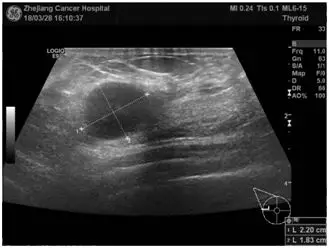
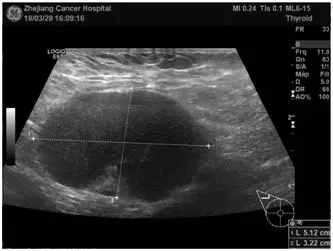
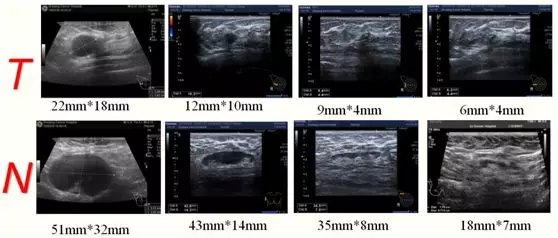
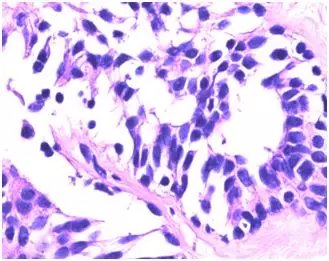
36岁,已婚。主诉:2018年3月28日因“发现右乳肿块半个月”入院。


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#进展期#
58
#新辅助#
43
#局部#
46
#三阴性#
45
学习谢谢分享
81