全髋关节置换术治疗脊髓痨性夏科氏髋关节病1例
2019-01-07 刘旭 实用骨科杂志
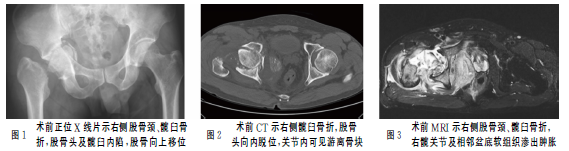
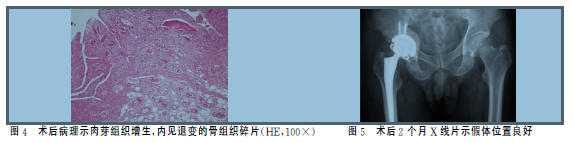
45岁男性患者,因右髋关节间歇性疼痛1年,摔倒后疼痛加重伴行走困难2周入院。既往史:2年前曾因“潜伏梅毒”行规范抗生素治疗。否认糖尿病、结核病病史,否认冶游史。查体:跛行步态,全身无皮疹,右下肢短缩外旋畸形,右髋部轻度肿胀,局部无瘢痕、窦道,右腹股沟中点、大转子轻度压痛,右侧髋关节被动活动范围基本正常,右下肢肌力Ⅳ级,深感觉减弱,右下肢生理反射减弱、病理反射未引出。骨盆正位X线片及髋关节CT示右侧
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#全髋关节#
38
#置换#
26
#脊髓痨#
37
#关节置换术#
35
#痨性夏科氏#
35
#置换术#
24