脉络丛肿瘤
概述
-
脑室内乳头状肿瘤, 起源于脉络丛上皮(WHO I级)
影像
见于儿童,脑室内分叶状肿块,伴显著强化
脉络丛乳头状瘤(CPPs) 的发生和正常脉络丛数量有关
-
50%位于侧脑室
-
40%位于第四脑室和第四脑室侧孔
-
5%位于第三脑室(顶)
脉络丛动脉扩张供应侧脑室(三角区) CPPs
脑积水常见
主要的鉴别诊断
-
脉络丛癌
-
髓母细胞瘤
-
幕下室管膜瘤
-
脑室内转移瘤
-
脑膜瘤
-
生理性脉络丛扩张
临床要点
-
1岁以下儿童最常见的脑肿瘤
-
占1岁以内脑肿瘤的13.1%
-
7.9%的胎儿脑肿瘤由超声诊断
-
经脑脊液通路种植罕见
诊断纲要
-
2岁以下儿童发现脑室内肿块,考虑CPP
-
仅凭影像难以可靠鉴别CPP和脉络丛癌
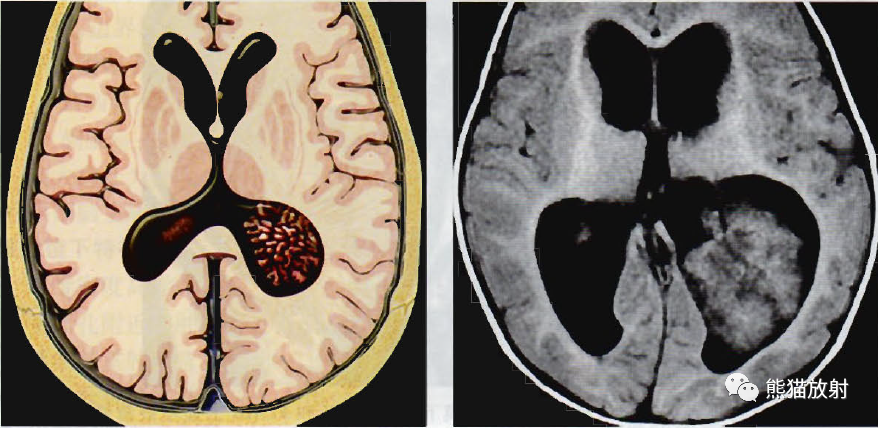
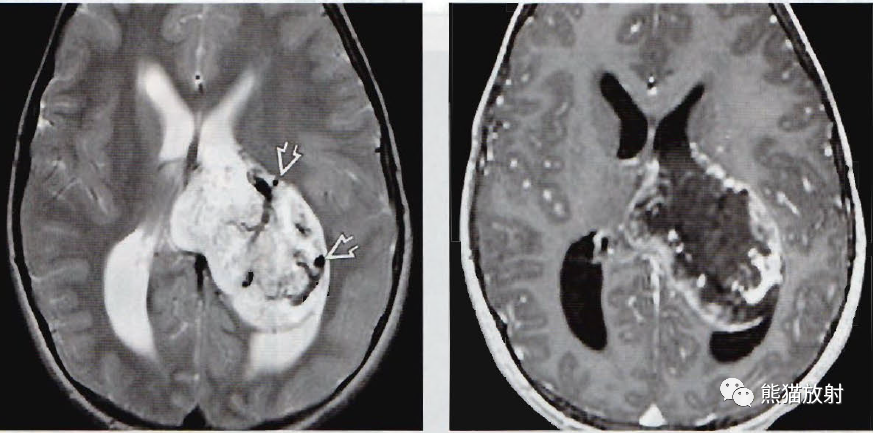
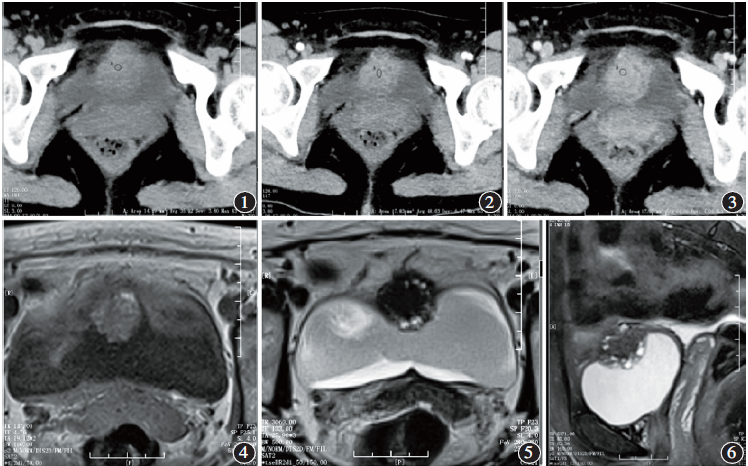
(左)轴位图显示一个起源于左侧脑室三角脉络丛的脉络丛乳头状瘤(CPP) 。注意肿瘤特征性的叶状表面突起,儿童CPP侧脑室最常见。
(右) 轴位T1WI显示18个月大儿童一个位于左侧脑室、呈分叶状的等信号肿块, 符合CPP的特点。注意伴发的脑积水,常和肿瘤分泌脑脊液过多有关。
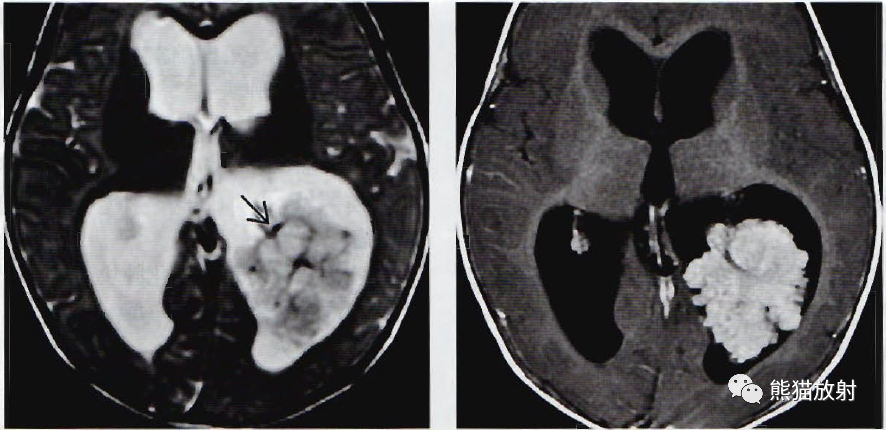
(左)轴位T2WI显示同一患者位于侧脑室的不均匀高信号肿块,散在低信号血管流空影,提示肿瘤血管丰富。临近脑实质无明显T2WI高信号, 提示局部无浸润生长。
(右) 轴位T1WI C+显示此分叶状肿瘤显著强化,伴肿瘤表面叶状突起,符合CPP特点。仅用传统影像学检查不能可靠鉴别CPP和脉络丛癌。
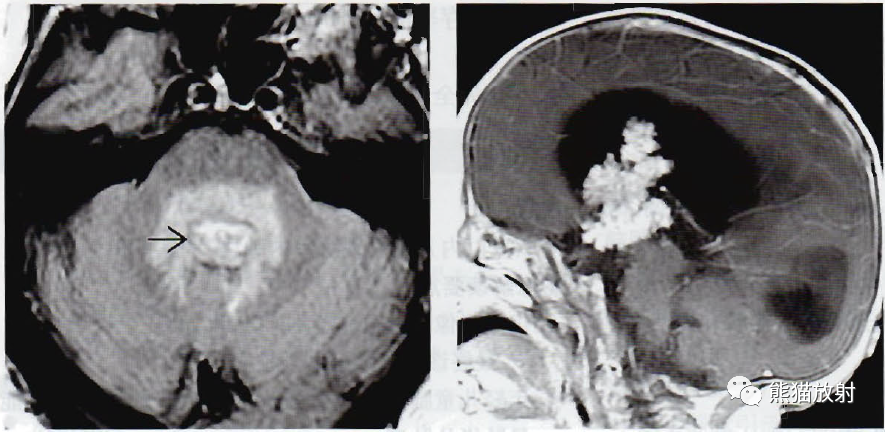
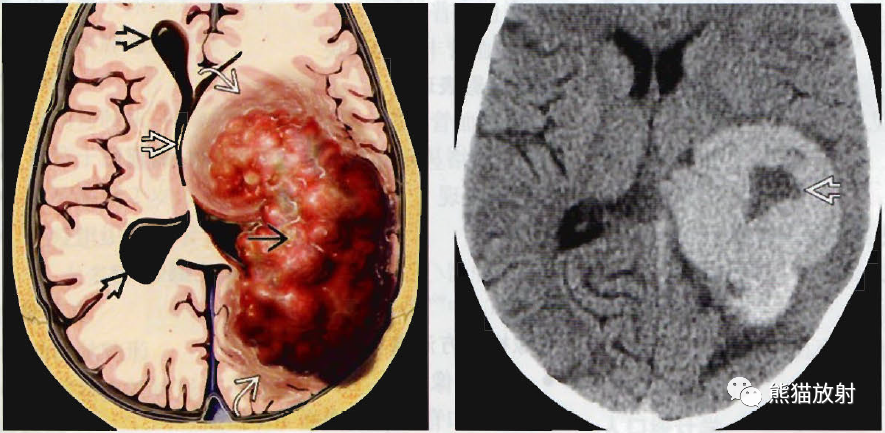
(左)52岁头痛、呕吐患者, 轴位FLAIR显示第四脑室高信号肿块,伴周围脑组织显著水肿,是WHO I级CPP非典型特征。该图像和非典型CPP或CPCa相似。
(右) 矢状位T1WI C+显示第三脑室显著强化的分叶状肿块,伴叶状突起,是脉络丛肿瘤少见发病部位。注意伴发的脑积水。
非典型脉络丛乳头状瘤
概述
-
脉络丛乳头状瘤(CPP) 伴有丝分裂活性增强和复发率增加(WHOⅡ级)
影像
-
儿童脑室内显著强化的分叶状肿块
-
可见出血和坏死
-
瘤内血管流空影常见
-
脑积水常见
-
影像学不能可靠的和脉络丛乳头状瘤(CPP) 或脉络丛癌(CPCa) 相鉴别
主要的鉴别诊断
-
CPP和CPCa
-
室管膜瘤
-
髓母细胞瘤
-
非典型畸胎样/横纹肌样瘤
病理
-
每10个高倍镜视野可见≥2个有丝分裂象:区分aCPP(WHOⅡ级) 和CPP(WHOⅠ级) 的唯一镜下标准;与复发增加相关的最重要因素
-
非典型特征增加:高细胞密度,细胞核多形性,坏死,实性生长
-
可表现为Ki-67和MIB-1增殖指数升高
临床要点
-
巨颅畸形和呕吐最常见
-
手术完全切除一般可治愈
-
非典型CPP的复发率是WHO I级CPP的4.9倍
-
5年生存率接近100%
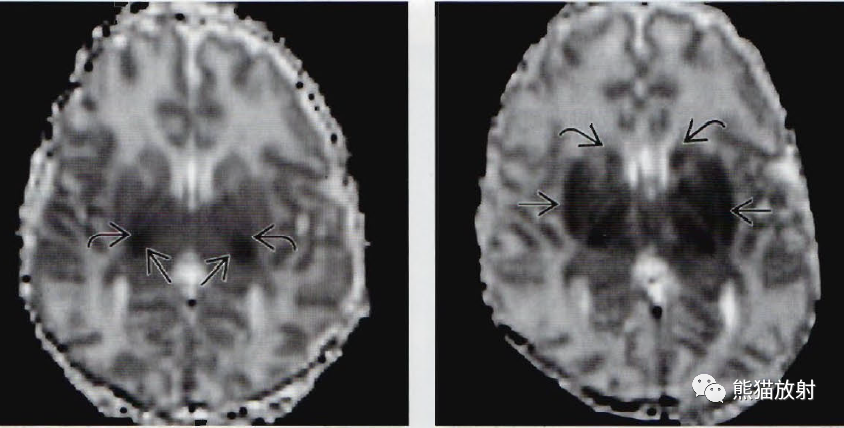
(左)轴位T2WI显示第三脑室不均匀高信号肿块回,向上通过室间孔扩展到侧脑室,穹隆柱向前上倾斜,以此确定肿瘤起源于第三脑室。注意侧脑室明显扩张。
(右) 冠状位T1WI C+显示同一患者一个分叶状,显著强化的肿块,此为脉络丛肿瘤的特点,手术证实为WHOⅡ级肿瘤。
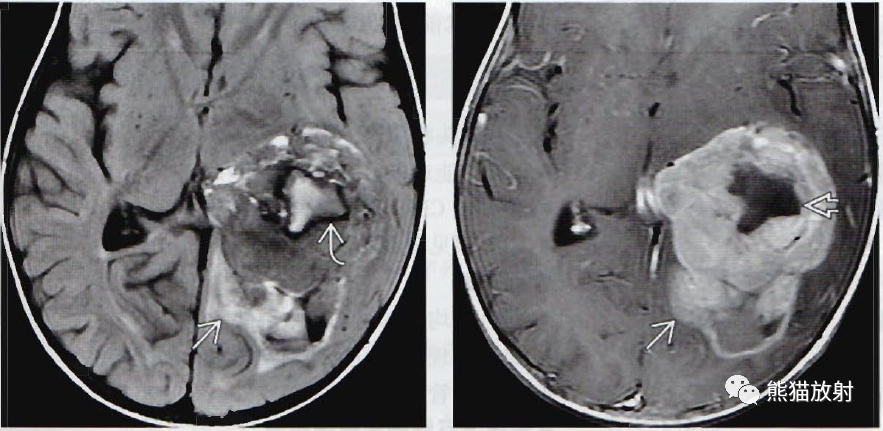
(左)轴位T2WI显示15岁头痛伴视乳头水肿患者脑室内高信号肿块,伴明显血管流空影和脑水肿。
(右)轴位TIWI C+图像显示该患者肿瘤周围强化, 中央区无强化提示肿瘤坏死。手术证实为WHOⅡ级非典型CPP。这些罕见的肿瘤可有和典型Ⅰ级CPP相似的表现或表现为不典型的影像学特征, 此例即如此。
脉络丛乳头状癌
概述
-
起源于脉络丛上皮的恶性肿瘤(WHOⅢ级)
影像
-
最佳诊断要点:5岁以下,影像学发现可强化的脑室内肿块和室管膜浸润,伴或不伴显著的流空
-
非对称性脑室周围白质水肿提示浸润
-
MR可能难以区分乳头状瘤和脉络丛癌:信号不均匀, 脑实质浸润和脑脊液播散提示CPCa
-
术前行脊髓影像检查重要
主要的鉴别诊断
-
脉络丛乳头状瘤(CPP)
-
室管膜瘤
-
室管膜下巨细胞星形细胞瘤
病理
-
镜下特点:细胞密度高,细胞多形性,有丝分裂活跃
-
囊肿、坏死、出血、微钙化
-
脑实质浸润常见
-
Li-Fraumeni和Aicardi综合征发病率增加
临床要点
-
见于婴儿和年轻儿童,70%发病年龄小于2岁
-
恶心、呕吐、头痛、精神迟滞为最常见症状
-
CPCa占所有脉络丛肿瘤的20%~40%
-
生长迅速,5年生存率:30%~50%
-
有脑实质浸润或脑脊液种植者预后差
(左)轴位图显示一位于左侧侧脑室三角区中心的分叶状肿块。注意肿瘤浸润和周围脑组织肿胀必,更符合脉络丛癌的特点,导致中线移位,右侧脑室受压。
(右)2岁精神异常患儿,轴位NECT显示左侧脑室侧脑室三角区高信号肿块,伴坏死区。
(左) 同一患者,轴位FLAIR显示位于左侧侧脑室三角区中心的不均匀肿块,临近脑组织高信号提示脑组织浸润。注意低信号区和血液产物有关。
(右) 同一患者,轴位T1WI C+显示脑室内肿块显著强化,伴中央坏死。注意临近枕叶的强化,提示肿瘤浸润。手术证实为CPCa。
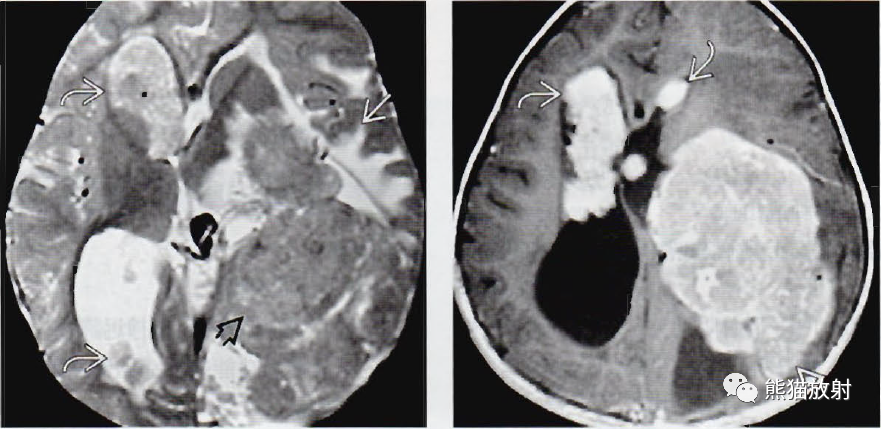
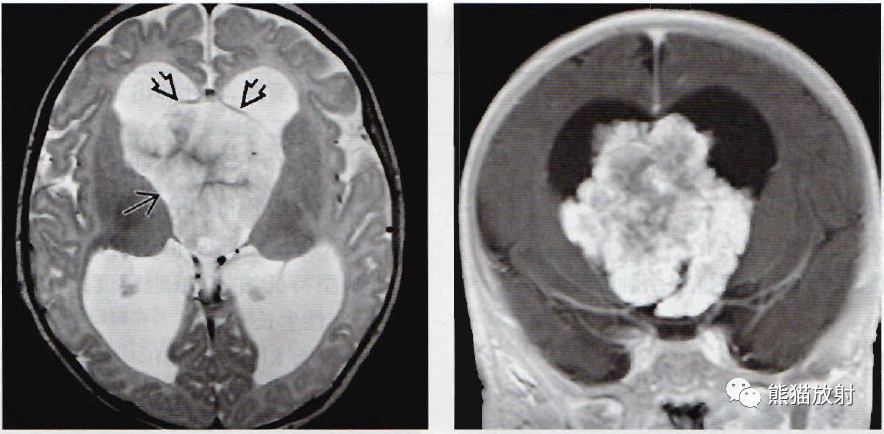
(左) 轴位T2WI显示位于左侧侧脑室的大块状脉络丛癌,伴脑脊液转移的多发结节。注意脑组织浸润相关的脑室周围不对称性T2WI高信号。
(右) 同一患者,轴位T1WI C+显示侧脑室脉络丛癌明显强化, 伴室管膜浸润和脑脊液播散的多发转移结节。脑脊液播散及脑实质浸润和预后差有关。
↓ 内容节选自图书:
 《脑部影像诊断学》 主译:吴文平 等
《脑部影像诊断学》 主译:吴文平 等
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#脉络丛#
0
#乳头状#
46
#影像诊断#
40
#诊断要点#
48