Br J Cancer:治疗后炎症相关生物标志物与结直肠癌患者生存之间的关联性研究
2021-07-09 xiaozeng MedSci原创
炎症反应在结直肠癌(CRC)的发生发展中起着至关重要的作用。
炎症反应在结直肠癌(CRC)的发生发展中起着至关重要的作用。慢性炎症与结直肠癌发生的关联性涉及了多种炎症因子。这些炎症调节因子包括肿瘤浸润免疫细胞和肿瘤细胞释放的细胞因子和趋化因子,其可以激活炎症反应并刺激肿瘤的生长。
既往研究显示,肥胖引起的低度全身炎症可通过改变脂肪因子的水平促进结直肠癌的发生和肿瘤的生长。因此,这些源自肿瘤微环境或脂肪组织的炎症生物标志物的失调可能会影响CRC的最终结局,且可能有助于识别疾病的进展以及筛选死亡风险较高的CRC患者。
该研究共纳入了来自西雅图结肠癌家族登记处的306例符合条件的II-III期CRC病例。研究人员测量了治疗后的患者血浆样品中的C反应蛋白(CRP)、白细胞介素6(IL-6)、单核细胞趋化蛋白1(MCP-1)、脂联素(adiponectin)和瘦素(leptin)的浓度。并通过Cox比例风险回归模型计算患者的全因死亡率和CRC特异性死亡率的调整后风险比(HR)和95%置信区间(CI)。
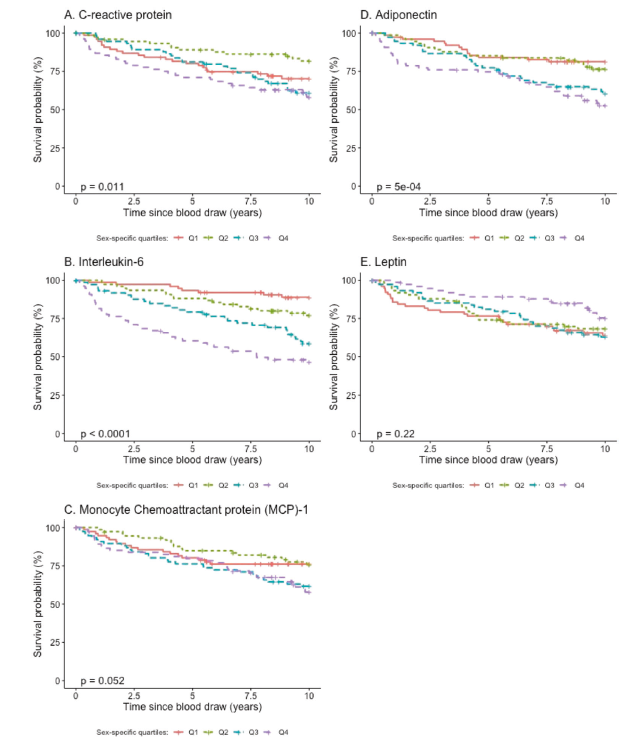
结果显示,CRP、IL-6、MCP-1和脂联素的水平升高与患者抽血后的10年内的全因死亡率升高风险显著相关,HR分别为1.32、2.72、1.97和1.71。研究人员发现,IL-6和脂联素具有剂量反应效应。
进一步的研究发现,在抽血后的第一年年内,CRP、IL-6、MCP-1以及脂联素与CRC特异性死亡率呈正相关,而瘦素则呈负相关,而IL-6的关联性则在10年里仍具有统计学意义。
Kaplan–Meier生存曲线分析
总而言之,该研究结果主要阐述了慢性炎症在CRC发生发展中的作用,而上述的几种治疗后炎症生物标志物,特别是IL-6,或可成为II-III期CRC患者的潜在的预后标志物。
原始出处:
Hua, X., Kratz, M., Malen, R.C. et al. Association between post-treatment circulating biomarkers of inflammation and survival among stage II–III colorectal cancer patients. Br J Cancer (06 July 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#患者生存#
41
#标志物#
39
#结直肠#
39
#生物标志#
43
#生物标志#
41
非常感谢
53