Prostate: 中国老年男性良性前列腺增生患者的前列腺形态学参数与临床进展的相关性研究
2021-04-30 AlexYang MedSci原创
最近,有研究人员调查了中国老年男性的前列腺形态学参数与良性前列腺增生(BPH)临床进展的相关性情况。
最近,有研究人员调查了中国老年男性的前列腺形态学参数与良性前列腺增生(BPH)临床进展的相关性情况。
研究是一项回顾性研究中,共包括了1038名患者。通过经直肠超声(TRUS)测量了前列腺形态。记录了所有候选人的详细病史,并根据具体的前列腺测量结果进行了分类分析,并采用单变量和多变量的逻辑回归分析评估了变量之间的相关性。
研究结果发现,研究人群中BPH临床进展的累积发生率为63.68%(661/1038)。前列腺体积(PV)、过渡区体积(TZV)、过渡区指数(TZI)和膀胱内前列腺突起(IPP)均与BPH进展呈正相关(所有P<0.001)。PV>60ml、TZV>15ml、TZI>0.5或IPP>5mm的患者,整体BPH临床进展的可能性明显较高(调整后的OR:分别为2.485、1.678、1.886和1.924;95%CI:1.559-3.960、1.131-2.489、1.379-2.579和1.357-2.728)。
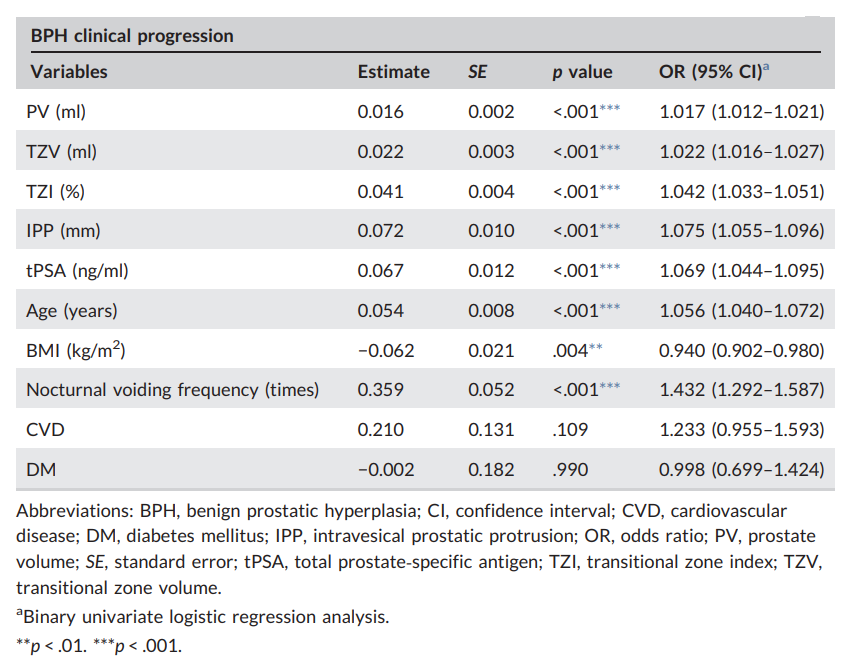
BPH临床进展相关因素的单变量分析
最后,研究人员指出,前列腺形态学参数与前列腺增生症的临床进展显著相关。前列腺形态学参数较大的患者更容易出现临床进展。因此,在临床进展发生之前,应及时考虑对这些患者进行合理的治疗。
原始出处:
Subo Qian, Shun Zhang, Weimin Xia et al. Correlation of prostatic morphological parameters and clinical progression in aging Chinese men with benign prostatic hyperplasia: Results from a cross-sectional study. Prostate. Apr 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#老年男性#
61
#相关性#
51
#ROS#
50
#良性前列腺增生#
49
#PRO#
35