Rheumatology:新诊断系统性红斑狼疮患者脑白质微结构的纵向变化
2021-06-27 MedSci原创 MedSci原创
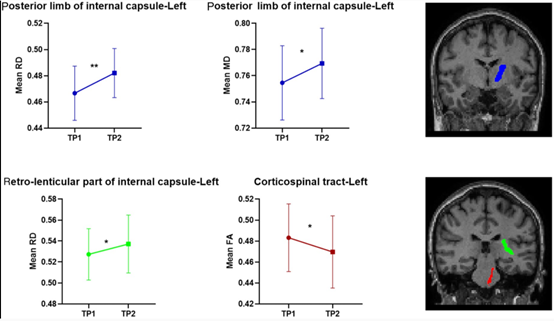
在SLE病程的初始阶段,即使没有明显的神经精神(NP)症状,扩散系数的增加也反映了WM组织微结构的受损。
系统性红斑狼疮(SLE)是一种自身免疫性疾病,其特点是多器官受累,临床表现广泛,包括神经精神综合征(NP)。NP综合征影响中枢和外周神经系统,影响疾病结果以及患者的生活质量。SLE病程初始阶段的患者NP受累的风险很高。目前,由于缺乏预测这些并发症的特异性生物标志物,或由于无法将其归因于SLE,无法确定SLE患者以后会发展为NP综合征。缺乏可靠的疗效指标进一步阻碍了对疾病的有效监测和治疗效果的评估。因此,寻找与SLE患者NP参与相关或允许监测疾病进展的结果指标是该领域最重要的未满足需求之一。 Ettore Silvagni等评价了SLE患者不同脑白质(WM)束弥散张量成像(DTI)指标的纵向变化,并评价DTI变化是否与临床特征随时间的变化有关。研究结果发表在Rheumatology杂志。 对17例初治SLE患者(19-55岁)在确诊后24个月内进行基线脑部MRI(1.5T Philips Achieva)评估和至少12个月后再评估。计算了几个正常出现的WM域的分数各向异性、平均扩散系数(MD)、径向扩散系数(RD)和轴向扩散系数。采用重复测量方差分析法对DTI指标的纵向变异进行分析。对2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#新诊断#
33
#系统性#
37
#Rheumatology#
29
#微结构#
36
#白质#
26
#狼疮#
26
#红斑#
29
👍👍
67