Aging Cell:清除全身衰老细胞可缓解脑部炎症和认知功能障碍
2021-01-21 haibei MedSci原创
在神经退行性疾病的小鼠模型中,清除衰老细胞已被证明可以改善大脑功能。然而,衰老细胞的清除是否能缓解衰老过程中的认知功能障碍仍是未知数。
已有的研究显示,衰老过程的特点是记忆力、注意力控制力、定向力和认知力的逐渐下降。此外,衰老是一些神经退行性疾病发展的主要风险因素,如肌萎缩侧索硬化症(ALS)、原发性进行性多发性硬化症(PPMS)、阿尔茨海默病(AD)和帕金森病(PD)。
细胞衰老的特点是不可逆的细胞周期停滞和促炎性衰老相关分泌表型(SASP),这是衰老和年龄相关疾病的主要因素。在神经退行性疾病的小鼠模型中,清除衰老细胞已被证明可以改善大脑功能。然而,衰老细胞的清除是否能缓解衰老过程中的认知功能障碍仍是未知数。
为了研究这个问题,研究人员首先在年轻和老年小鼠的海马中进行了单核和单细胞RNA-seq。其观察到p16Ink4a衰老细胞的年龄依赖性增加,这在小胶质细胞和少突胶质细胞祖细胞中更为明显,衰老细胞具有分泌SASP的特征。
然后,研究人员对INK-ATTAC小鼠进行了老化处理,并用AP20187或清除衰老细胞的鸡尾酒疗法Dasatinib和Quercetin进行处理。研究人员观察到,这两种策略都导致p16Ink4a在小胶质群体中特异性减少,导致小胶质激活减少,SASP因子表达减少。
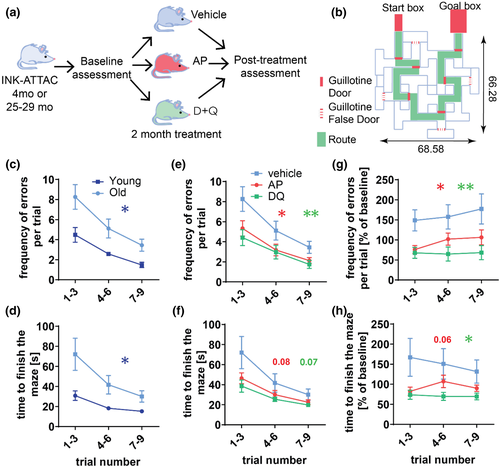
重要的是,这两种方法都能显著改善老年小鼠的认知功能。
因此,该数据为清除衰老细胞干预成为缓解年龄相关认知障碍的潜在治疗途径提供了概念证明。
原始出处:
Mikolaj Ogrodnik et al. Whole‐body senescent cell clearance alleviates age‐related brain inflammation and cognitive impairment in mice. Aging Cell (2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cell#
36
#CEL#
25
学习了,
68
👍
82
#功能障碍#
33