JACC:脂蛋白(a)和冠脉钙化与动脉粥样硬化心血管风险的独立相关性
2022-03-09 xiaozeng MedSci原创
脂蛋白(a) 和冠状动脉钙化评分与动脉粥样硬化性心血管疾病的风险独立相关
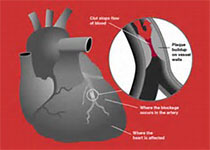
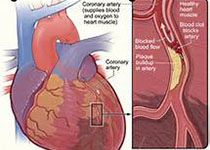
脂蛋白(a) [Lp(a)]升高和冠状动脉钙化 (CAC) 评分均与动脉粥样硬化性心血管疾病 (ASCVD) 风险增加独立相关,但目前尚未进行过联合研究。
本研究目的是调查脂蛋白(a)和冠状动脉钙化评分与动脉粥样硬化性心血管疾病风险的独立及联合相关性。
MESA(动脉粥样硬化的多种族研究)队列(n=4512)和DHS(Dallas心脏研究)队列(n=2078)招募的无症状受试者在入组时检测了血浆脂蛋白(a) 水平,并评估了冠状动脉钙化评分。Lp(a) 升高定义是种族特异性的最高的五分位;根据冠状动脉钙化评分又将受试者分成了三组:0分、1-99分、≥100分。采用危险因素调整的Cox回归模型评估Lp(a)和冠状动脉钙化与动脉粥样硬化性心血管疾病的相关性。
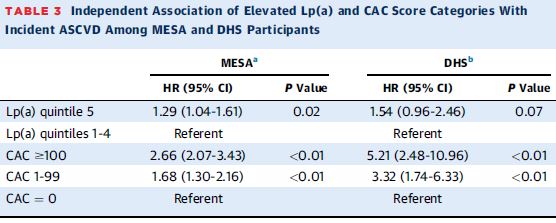
在两个队列中,Lp(a)和CAC评分与ASCVD风险的相关性
在MESA队列受试者(平均61.9岁,52.5%的女性,36.8%的白人,29.3%的黑人,22.2%的西班牙人,11.7%的中国人)中,中位随访 13.2 年期间共观察到了476例冠状动脉粥样硬化性心血管疾病。Lp(a) 升高和冠状动脉钙化评分(1-99分和≥100分)均与动脉粥样硬化性心血管疾病风险独立相关(HR分别是1.29、1.68和2.66)。Lp(a) 和冠状动脉钙化评分之间无相互作用。
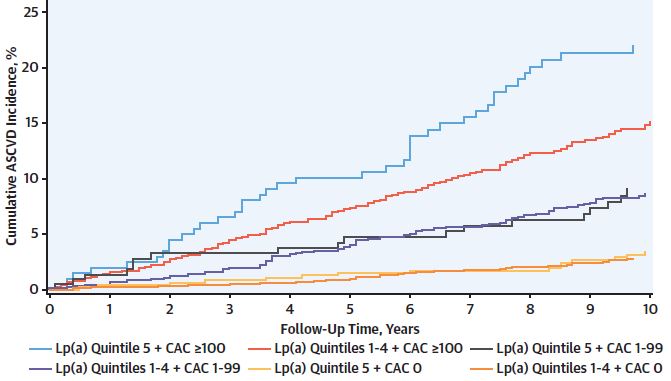
不同分组个体ASCVD的累积发生率
与Lp(a) 未升高和冠状动脉钙化 0分的受试者相比,Lp(a) 升高和冠状动脉钙化评分≥100分的受试者发生动脉粥样硬化性心血管疾病的风险最高(HR 4.71),但Lp( a) 升高和冠状动脉钙化评分为0分的受试者的患病风险无明显升高(HR 1.31)。在DHS队列中观察到了相似的结果。
综之,脂蛋白(a) 和冠状动脉钙化评分与动脉粥样硬化性心血管疾病的风险独立相关,有望同时用于指导动脉粥样硬化性心血管疾病的初级预防治疗决策。
原始出处:
Mehta Anurag,Vasquez Nestor,Ayers Colby R et al. Independent Association of Lipoprotein(a) and Coronary Artery Calcification With Atherosclerotic Cardiovascular Risk.[J] .J Am Coll Cardiol, 2022, 79: 757-768. https://doi.org/10.1016/j.jacc.2021.11.058
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JACC#
50
#粥样硬化#
49
#血管风险#
47
#相关性#
40
#ACC#
51
#脂蛋白#
55
#冠脉钙化#
48