Interact Cardiovasc Thorac Surg:阜外医院郑哲发现房颤伴左房扩大,外科微创消融双房更有效!
2022-03-19 中国循环杂志 网络
治疗晚期阵发性房颤或持续性房颤,胸腔镜下双房消融(BA Lesion)比“盒式”(Box lesion)消融更有效,能减少房性快速心律失常复发。
以往有研究显示,胸腔镜下射频消融术常以肺静脉或左心房后壁和左心耳为靶点,但消融局限,疗效有待提高。
电生理研究表明,右房可能在房颤机制中发挥重要作用。在阵发性或持续性房颤和左心房扩张的患者中,除左房外,右房基质可能参与房颤的发作和持续。
近期,中国医学科学院阜外医院郑哲等发表研究称,治疗晚期阵发性房颤或持续性房颤,胸腔镜下双房消融(BA Lesion)比“盒式”(Box lesion)消融更有效,能减少房性快速心律失常复发。
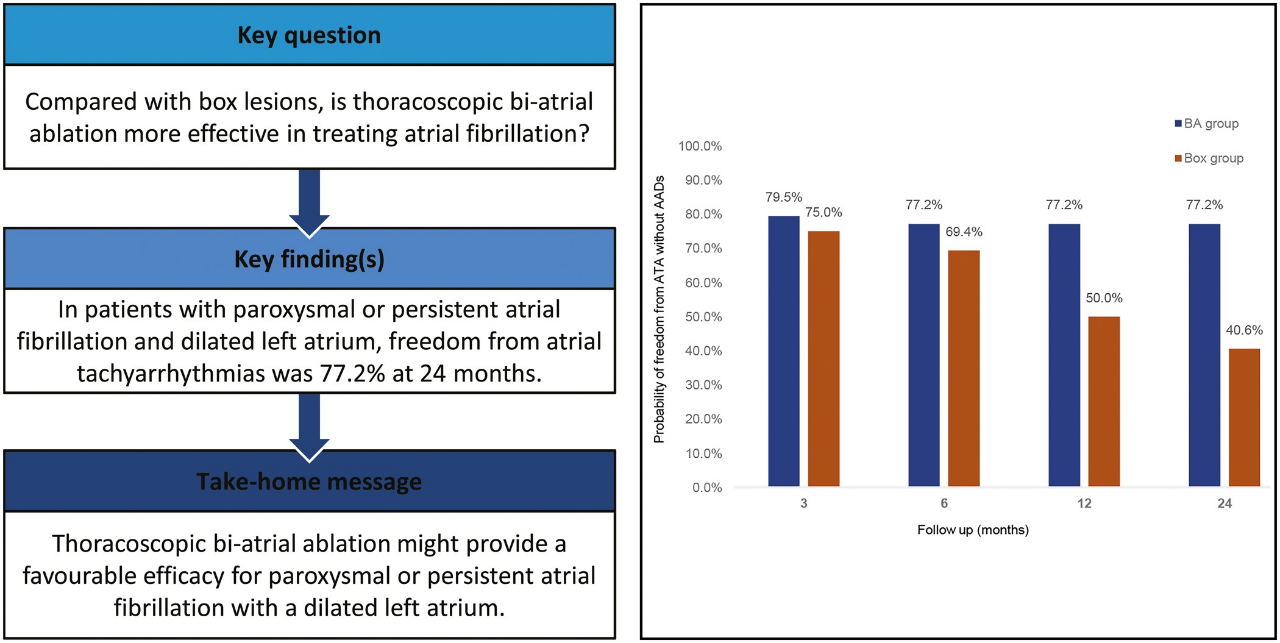
研究显示,双房消融疗效明显优于盒式消融
研究纳入80例有左房扩大(左心房直径>40 mm)和导管消融失败的阵发性或持续性房颤患者。36例患者接受了胸腔镜心外膜“盒式”消融,44例患者接受了双房消融。

入组的患者中,双房消融组患者持续性房颤和三尖瓣反流更多(86.4% vs. 47.2%),左房也更大(48 mm vs. 42 mm)。两组患者组之间没有其他显著差异。
平均随访32个月,两组在手术并发症方面没有差异。
双心房消融组在6个月、12个月和24个月,在未服用抗心律失常药物情况下的无房性快速心律失常的比例分别为77.2%、77.2%和77.2%,而“盒式”消融组的比例逐渐下降,分别为69.4%、50.0%和40.6%。
研究者指出,尽管双房消融组患者有较大的左房和较多的三尖瓣反流,以及更多的持续性房颤,但房性快速心律失常仍较少发生,这意味着双房消融可能具有疗效优势。
双房消融组术后主要并发症是无症状的小肺栓塞。且没有植入永久性起搏器的情况,研究者分析,原因是右房消融时远离窦房结区;其次,双房消融组恢复窦性心律的患者也没有病态窦房结综合征。
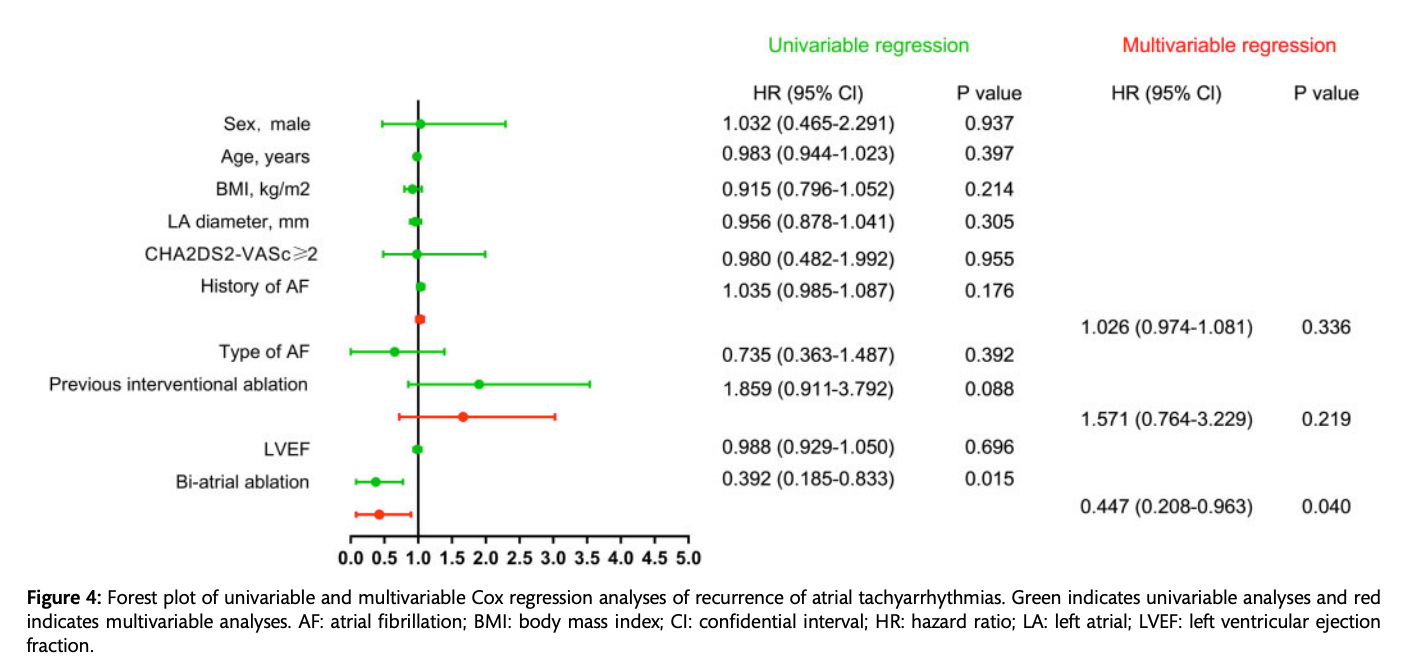
对性别、年龄、体重指数、左心房直径、房颤类型、房颤病史和既往介入消融术进行校正后进一步分析显示,双房消融使房性快速心律失常复发风险降低55%。
2020年欧洲心脏病学会房颤指南建议,对于有症状的阵发性或持续性房颤的患者,若抗心律失常药物治疗无效且介入房颤消融失败,或有明显介入射频消融失败高风险患者,胸腔镜手术消融是合理。
研究者预期,因手术创伤性小,胸腔镜下心外膜消融治疗无结构性心脏病的房颤将有应用前景。
原始出处:
Zheng Z, Li H, Liu S, Gao G, Yu C, Lin H, Meng Y. Box lesion or bi-atrial lesion set for atrial fibrillation during thoracoscopic epicardial ablation. Interact Cardiovasc Thorac Surg. 2022, 34(1):1-8.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#阜外医#
41
#ERA#
36
#ASC#
39
#THORAC#
37
#阜外医院#
62
#微创#
30
#消融#
51