J Clin Hypertens: 男性、年轻、吸烟、单药治疗影响高血压控制!王继光等对36.4万人的研究
2020-04-25 卢芳 中国循环杂志
我国每5个成年人中就有1人有高血压,而心血病死亡中,至少50%与高血压有关。
我国每5个成年人中就有1人有高血压,而心血病死亡中,至少50%与高血压有关。
但遗憾的是,高血压的控制还是不尽人意。
上海瑞金医院王继光等在36.4万人中进行的研究揭示:男性、年轻、当前吸烟、单药治疗都影响了高血压的有效控制。
这项大规模机会性筛查研究中,高血压知晓率为60.1%,治疗率42.5%,控制率25.4%,治疗控制率为59.8%。
研究显示,男性不论收缩压还是舒张压都高于女性。
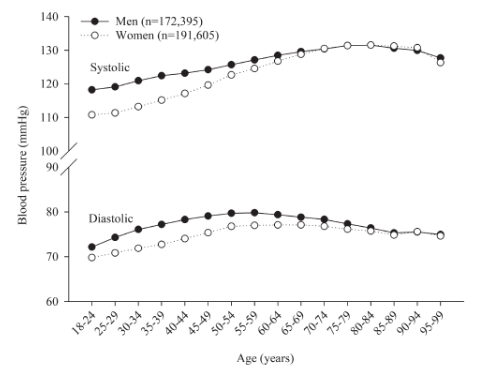
图1 不同年龄组男女平均收缩压和舒张压水平
而且,男性的高血压患病率也高于女性,这种男女差异主要是65岁以下人群促成,这一人群男性高血压患病率是女性的两倍。
但是,女性在知晓率、治疗率和控制率均高于男性,治疗控制率也比男性高一点。
此外,在有合并症的人群中,高血压的知晓率、治疗率和控制率均有所改善。
研究还发现,年龄大,有利于改善高血压的知晓和治疗,但是影响血压控制;吸烟督促知晓率有所提高,但影响治疗和控制;单用降压药不利于血压控制。
研究者强调,吸烟是高血压管理的重要的绊脚石,吸烟人群是高血压管理的目标人群。
一则吸烟的人高血压患病率会更高,其中包括隐匿性高血压;此外尽管吸烟者比不吸烟者知晓率高,但治疗率和控制率却都较低。
而且,吸烟多是男性的“顽疾”,这项研究中,男士有20.3%的人吸烟,而女性为1.9%。
另外一个重要的问题是降压药的使用问题,在这项研究中,尽管高血压控制率低,但联合用药并不充足,有73.3%的患者单一用药,联合用药比例仅26.7%。
研究者介绍,近期发布的高血压管理指南均一致推荐起始降压就联合用药。
考虑到依从性问题,我国已有很多单片的复方制剂可以使用。研究者指出,联合降压将是改善血压控制的重要手段。
针对“男性”和“年轻”,研究者认为,可能建立相关技术平台有助于针对性改善这两个人群的高血压问题,比如当前在办公环境、购物商场、飞机场、火车站等处在建的网页为基础或微信相关的血压管理系统。
研究者希望,通过这些平台对男性、年轻人的高血压管理有所促进。
这项研究纳入的36.4万人中,89.7%使用电子血压计,11.3%使用水银血压计量血压。
男士超重和肥胖更多见,饮酒的人也不在少数。男女糖尿病、冠心病、脑卒中及短暂性脑缺血发作,以及使用他汀的比例均相似。
原始来源:
Chen X, Xu SK, Guo QH, et al. Barriers to blood pressure control in China in a large opportunistic screening. J Clin Hypertens (Gree). 2020 Apr 9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PE#
42
#TENS#
37
#王继光#
50
#单药治疗#
37
#血压控制#
42