Bioorg Med Chem:羟氯喹抗SARS-CoV-2病毒,再现曙光!
2022-08-18 August MedSci原创 发表于上海
自 2019 年底以来,严重急性呼吸系统综合症冠状病毒 2(SARS-CoV-2)的爆发已演变为全球大流行。迫切需要有效且低毒的抗病毒药物来弥补瑞德西韦的局限性。
羟氯喹最早被发现,具有强烈抑制新冠病毒的作用,因此,一度被用于新冠疾病的治疗。世界卫生组织于 2020 年启动了一项名为“团结试验”的多国随机试验,以研究一些有希望的分子或药物组合对 COVID-19 的疗效。其子集包括瑞德西韦和羟氯喹。然而,羟氯喹的一些副作用限制了其使用,其安全性并不如瑞德西韦。最终各国不再推荐使用(羟)氯喹用于新冠病毒的治疗。
然而,开发针对新病毒的高效新药既昂贵又耗时。尽管已经发现了许多针对 SARS-CoV-2 不同靶点的小分子抑制剂,但面对迅速蔓延且日益严重的疫情,这些抑制剂并不能立即解决当前的困境。鉴于这些挑战,药物再利用可能是一种理想的策略。药物再利用具有许多优点,包括节省时间、金钱和临床经验保证安全。
那么羟氯喹是否有再挖掘的潜力呢?最新的研究,发现羟氯喹的两种不同的对映体作用不一样!为羟氯喹的使用再现曙光!
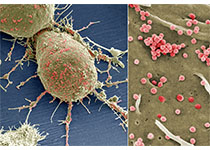
代表性的抗病毒药物和羟氯喹的对映体:
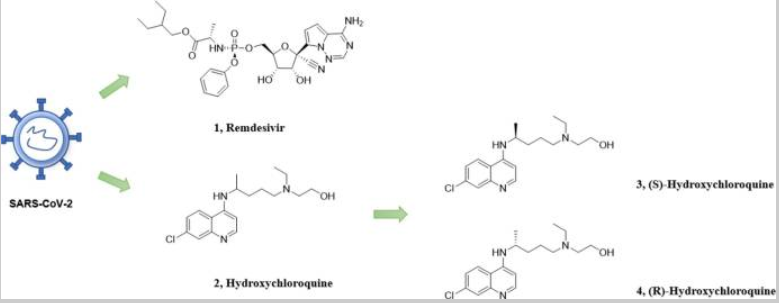
羟氯喹是一种广谱抗病毒药物,在一些研究中显示出对 SARS-CoV-2 的抑制活性。因此,有研究采用了药物再利用策略,并进一步研究了羟氯喹。利用手性拆分技术获得了不同构型的羟氯喹侧链,并通过化学合成成功得到了R-/S-硫酸羟氯喹。发现羟氯喹的 R 构型表现出更高的抗病毒活性 (EC50 = 3.05 μM) 和更低的体内毒性。而羟氯喹此前的研究结果显示,其抗新冠病毒的EC50在30μM左右。因此,R-HCQ 是一种很有前景的抗 SARS-CoV-2 的先导化合物。此研究为后续针对SARS-CoV-2的小分子抑制剂的研究提供了新的策略。
羟氯喹及其对映体的初步生化评价:
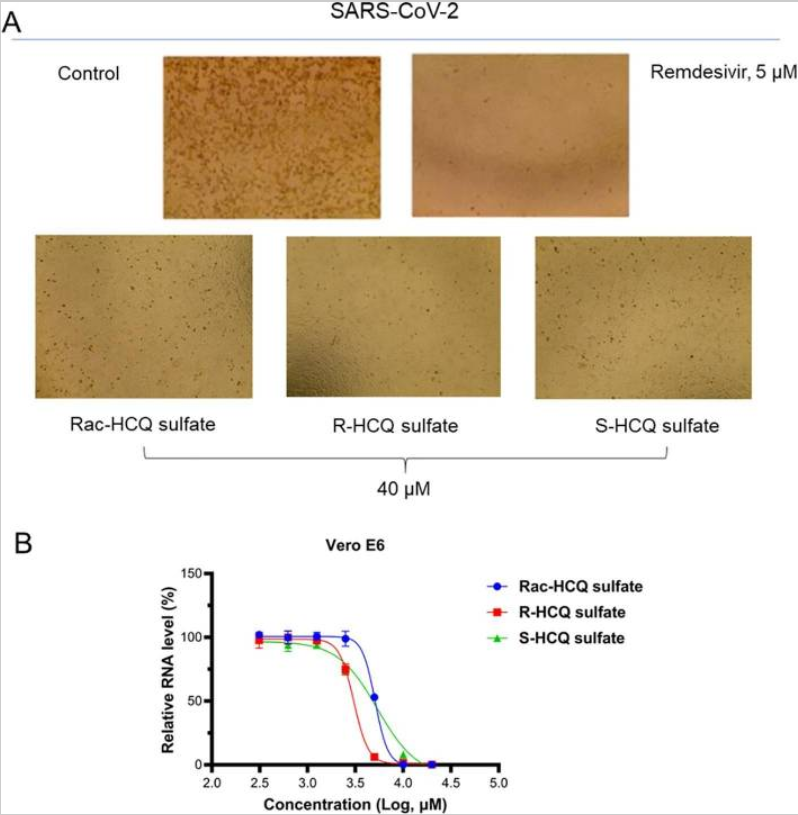
为了检查这三种化合物对去除病毒 RNA 的影响,研究者进一步测试了细胞上清液中病毒 RNA 的水平。与上述结果一致,这三种药物均显示出对病毒复制的有效抑制作用。其中,R-HCQ表现出最强的抑制活性(EC 50 = 3.05 μM),而外消旋体中羟氯喹的抑制水平(EC 50 = 5.09 μM)和S构型(EC 50 = 5.38 μM)具有可比性。这些数据表明,R-HCQ 可能是羟氯喹对 SARS-CoV-2 最有效的对映异构体之一。
小鼠在急性毒性试验中的存活曲线:

通过手性拆分和化学合成,成功合成了光学纯的羟氯喹。其中,R构型羟氯喹比S构型和外消旋羟氯喹表现出更高的抗病毒活性(EC 50 = 3.05 μM)。体内急性毒性试验表明,S-羟氯喹对消旋体的毒性较高,而R构型的毒性较低。R-羟氯喹的体内毒性优于 S-羟氯喹。基于以上内容,R-HCQ的合成及其生物学功能可能是推动该领域的重要启示。综上所述,R-HCQ 可能是进一步研究针对 SARS-CoV-2 的抗病毒药物的有前途的先导化合物。
参考文献:
Ni Y, Liao J, Qian Z, Wu C, Zhang X, Zhang J, Xie Y, Jiang S. Synthesis and evaluation of enantiomers of hydroxychloroquine against SARS-CoV-2 in vitro. Bioorg Med Chem. 2022 Jan 1;53:116523. doi: 10.1016/j.bmc.2021.116523. Epub 2021 Nov 22. PMID: 34875467; PMCID: PMC8606320.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#曙光#
48
#Bio#
53
#SARS-CoV#
51
#SARS#
49
#Med#
32