Diabetologia:新冠肺炎后新诊断糖尿病的发病率
2022-04-30 从医路漫漫 MedSci原创
新型冠状病毒可能通过触发促炎细胞因子来损伤β细胞。导致脂肪组织慢性低级别炎症的促炎途径在胰岛素抵抗和2型糖尿病的发病中发挥重要作用。
背景:人类胰腺是严重急性呼吸综合征冠状病毒2(新型冠状病毒)攻击的目标。新型冠状病毒感染后,观察到β细胞中胰岛素分泌颗粒的数量减少,葡萄糖刺激的胰岛素分泌受损。新型冠状病毒可能通过触发促炎细胞因子来损伤β细胞。导致脂肪组织慢性低级别炎症的促炎途径在胰岛素抵抗和2型糖尿病的发病中发挥重要作用。因此,在没有糖尿病病史的冠状病毒病患者中,已报告新发高血糖和胰岛素抵抗-2019(新冠肺炎)。然而,尚不清楚这种代谢改变是否是短暂的,或者个体是否会增加未来持续糖尿病的风险。
目的:这项工作的目的是调查感染冠状病毒疾病后的糖尿病发病率-2019(新冠肺炎)。患有急性上呼吸道感染(AURI)的个体,其经常由病毒引起,被选作非暴露对照组。
方法:我们使用疾病分析仪进行了一项回顾性队列分析,该疾病分析仪由德国各地1171名医师的代表性小组组成(2020年3月至2021年1月:880万患者)。新诊断的糖尿病根据ICD-10编码(二型糖尿病:E11其他形式的糖尿病:E12–E14)在随访期间,直到2021年7月(新冠肺炎的中位数为119天;AURI的中位数为161天。对性别、年龄、健康保险、新冠肺炎/AURI指数月和共病(肥胖、高血压、高脂血症、心肌梗死、中风)进行倾向评分匹配(1:1)。排除索引日期后30天内使用皮质类固醇的个体。泊松回归模型被拟合以获得糖尿病的发病率比率(IRRs)。
结果:在研究期间,共有35,865名新冠肺炎患者。在倾向评分匹配后,35,865名AURI对照者的人口统计学和临床特征相似(平均年龄43岁;46%女性)。与AURI相比,新冠肺炎患者的二型糖尿病发病率增加(15.8比12.3/1000人-年)。使用边际模型解释配对观察的相关性,估计二型糖尿病的IRR为1.28 (95% CI 1.05,1.57)。其他形式的糖尿病的IRR没有增加。
表1新冠肺炎或急性上呼吸道感染后新诊断糖尿病的发病率和发病率比率(AURI)
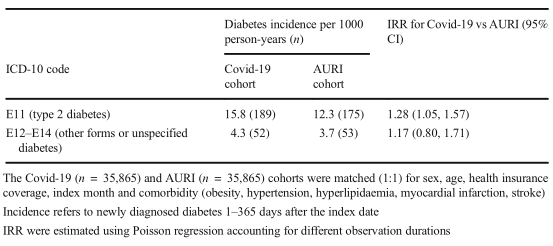
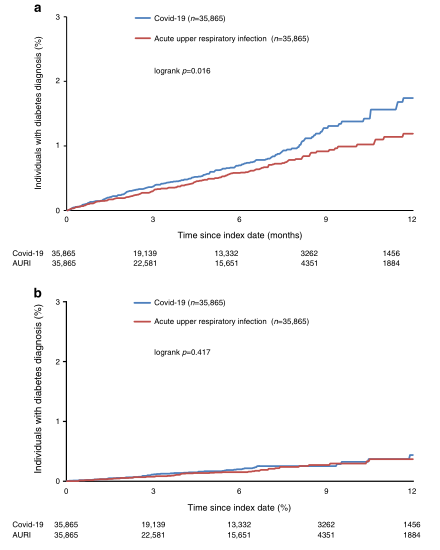
图1在DA初级保健数据库中匹配的Covid19和AURI个体中新诊断的糖尿病的Kaplan-Meier曲线:(a)二型糖尿病(E11),(b)其他形式的糖尿病(E12-14)。性别、年龄、健康保险覆盖范围、指数月和并发症(肥胖、高血压、高脂血症、心肌梗死、中风)的倾向评分匹配(1:1)
结论:新冠肺炎会增加患2型糖尿病的风险。如果得到证实,这些结果支持在轻度严重急性呼吸综合征冠状病毒2(SARSCoV-2)感染康复后应积极监测血糖,避免血糖调节紊乱。
原文出处: Rathmann W, Kuss O, Kostev K,Incidence of newly diagnosed diabetes after Covid-19.Diabetologia 2022 Mar 16
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#DIA#
43
#发病率#
31
#BET#
41
#新诊断#
40