Am Heart J: “功能性血运重建”理念迈出坚实一步!
2020-02-29 循环 中国循环杂志
美国心脏杂志(American Heart Journal)2020年2月24日在线发表了中国医学科学院阜外医院宋雷教授与上海交通大学涂圣贤教授为共同第一作者,中国医学科学院阜外医院徐波教授与乔树宾教授为共同通讯作者的题为“Quantitative flow ratio-guided strategy versus angiography-guided strategy for percutane
美国心脏杂志(American Heart Journal)2020年2月24日在线发表了中国医学科学院阜外医院宋雷教授与上海交通大学涂圣贤教授为共同第一作者,中国医学科学院阜外医院徐波教授与乔树宾教授为共同通讯作者的题为“Quantitative flow ratio-guided strategy versus angiography-guided strategy for percutaneous coronary intervention: Rationale and design of the FAVOR III China trial”的研究设计论文[1],是这项国人主持的高水平心血管病临床研究在成功完成全部患者的随机入组后,又一实质性进展。
“功能性血运重建治疗”始终是冠心病领域的研究热点与关键性问题。精准高效的识别那些干预价值高、真正造成心肌缺血的病变,有助于制定更加合理的治疗策略,切实改善患者的远期预后。
徐波教授团队在JACC 发表的FAVOR II China研究证实,以血流储备分数(FFR)作为判断冠脉狭窄生理学意义的金标准,QFR与前者的诊断一致性高达92.7%,为在线冠脉狭窄功能学评估提供了新方法,充分验证了QFR检测的高诊断精度、计算的便利性和经济性[2]。
FAVOR III China是由国家心血管病中心、中国医学科学院阜外医院发起(乔树宾教授和徐波教授担任主要研究者),全国26家著名心脏中心共同完成的,大规模、多中心、盲法(受试者和临床评价者设盲)、随机对照临床试验(Clinicaltrial.gov注册号NCT03656848),旨在接受介入治疗的冠心病人群中比较QFR指导与传统造影指导的远期临床结果与经济学效益。
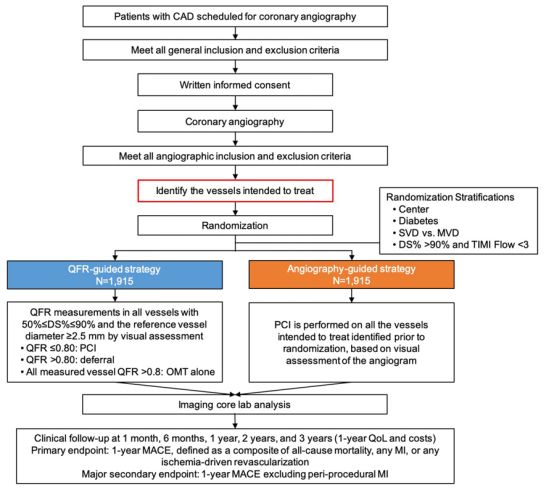
该试验是世界上首项用基于冠脉造影的功能学检测手段指导治疗的随机对照临床试验,在设计阶段即受到国内外相关领域专家的高度认可与关注,其结果将决定所有类似的功能学评价技术今后的临床地位,极有可能改写现行的临床指南。
研究同时得到了上海交通大学-博动医学影像联合实验室、复旦大学公共卫生学院等机构的高水平技术支持。
研究已于2020年1月如期完成全部受试者的随机入选,正在严格按计划进行为期3年的临床随访,其1年主要研究终点的结果将于2021年9月公布。
该研究的顺利实施将在ISCHEMIA试验[3]结果公布后,极大地推动“功能性血运重建”理念的应用,为冠脉血运重建的合理治疗决策提供有力证据;还将可能为有效管控医疗费用的不合理快速增长,制定合理的卫生政策提供依据,切实推动健康中国建设,真正惠及广大患者。
原始出处:
Song L, Tu S, Sun Z, Wang Y, Ding D, Guan C, et al. Quantitative flow ratio-guided strategy versus angiography-guided strategy for percutaneous coronary intervention: Rationale and design of the FAVOR III China trial. Am Heart J, In press, Available online 24 February 2020.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#功能性#
36
#功能性血运重建#
35
#ART#
29
#HEART#
37