JBC:在白血病细胞中靶向致癌酪氨酸磷酸酶SHP2的新型呋喃苯甲酰胺抑制剂的发现
2021-12-16 MedSci原创 MedSci原创
SBI-2130、SBI-4668和相关类似物可能不与催化口袋中的磷酸盐结合环结合。
在白血病细胞中靶向致癌酪氨酸磷酸酶SHP2的新型呋喃苯甲酰胺抑制剂的发现,已知由蛋白酪氨酸激酶 (PTK) 和蛋白酪氨酸磷酸酶 (PTP) 控制的信号分子酪氨酸磷酸化和去磷酸化之间的动态平衡紊乱,被认为会导致癌症的发展。
虽然大多数批准的靶向癌症疗法是酪氨酸激酶抑制剂,但 PTP 长期以来一直被认为是不可成药的,并且直到最近才在药物发现中重新受到关注。一个 PTP 目标是含有 Src 同源 2 结构域的磷酸酶 2 (SHP2)。SHP2 与肿瘤的发生、进展、转移和治疗抵抗有关,主要是因为它作为细胞外信号调节激酶 (ERK) 通路的信号连接,作用于小 GTPase Ras 的上游。
开发靶向SHP2的小分子的努力正在进行中,几种SHP2变构抑制剂目前正在用于治疗实体肿瘤的临床试验中。然而,虽然报道的变构抑制剂对表达野生型(WT)SHP2的细胞非常有效,但没有一种对最常见的致癌SHP2变异具有显著活性,这些变异驱动了一些青少年和急性白血病的白血病发生。
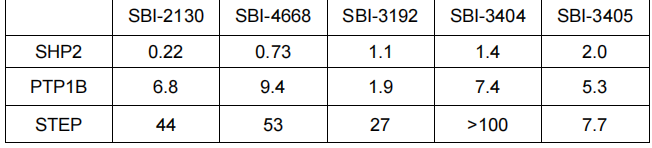
表:呋喃苯甲酰胺抑制剂对SHP2对相关磷酸酶PTP1B和STEP的选择性(半抑制浓度值为M;每个PTP结构由催化域组成)
在这里,研究团队报告了作为 WT 和致癌 SHP2 抑制剂的新型呋喃基苯甲酰胺分子的发现。重要的是,这些抑制剂很容易穿过细胞膜,在生理条件下结合和抑制 SHP2,并有效地减少癌细胞的生长,包括三阴性乳腺癌 (TNBC) 细胞、表达 WT 或致癌 SHP2 的急性髓性白血病 (AML) 细胞和患者来源的 AML 细胞。
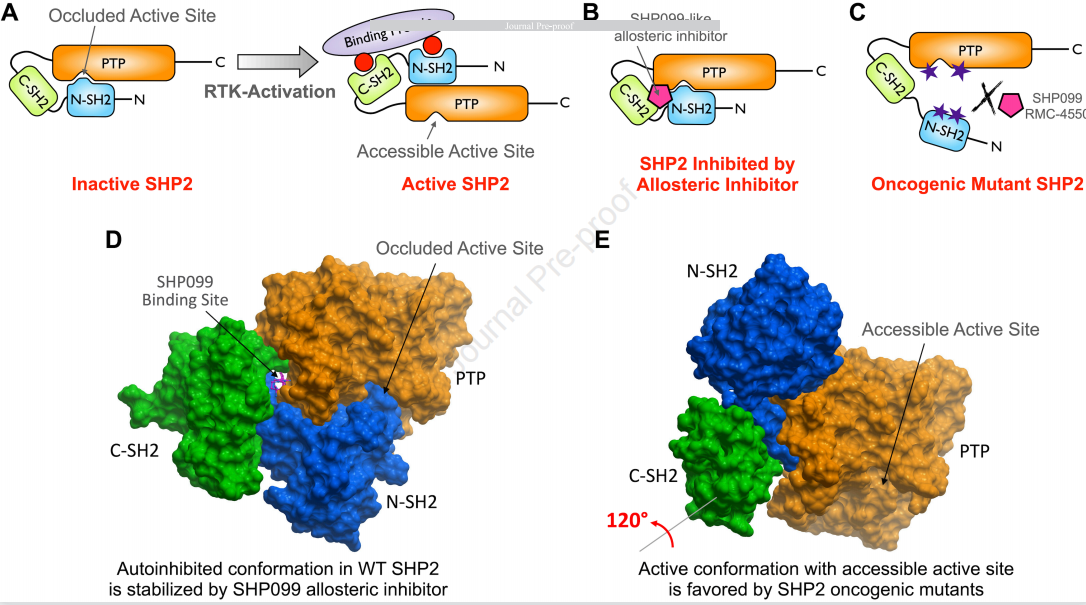
图1:SHP2的调控、抑制和致癌突变。SHP2激活的A)模型。受体酪氨酸激酶(RTK)的激活通过其两个SH2结构域通过酪氨酸磷酸化基序招募SHP2,导致构象从“封闭”、自抑制到“开放”、活跃的构象。变构抑制剂如SHP099抑制SHP2的B)模型。这些“分子胶”型化合物稳定了SHP2的非活性封闭构象。C)SHP2致癌变异激活的共同机制模型。N-SH2/PTP结构域界面上的单个氨基酸突变阻止了这两个结构域的分子内结合,从而形成了具有构成型活性的SHP2。变构抑制剂如SHP099和RMC-4550不能结合SHP2获得功能突变体首选的开放构象。D)野生型SHP2的晶体结构代表封闭的、自抑制的构象,如A)所述(PDBID:5EHR)。N-SH2结构域,蓝色;C-SH2结构域,绿色;PTP结构域,橙色;变构抑制剂SHP099(洋红色,棒状表示)与PTP、N-SH2和C-SH2结构域形成的通道结合,并稳定非活性构象,如B所述)。E)SHP2E76K功能获得突变体的开放、活性构象的晶体结构(PDBID:6CRF)。为了采用这种构象,C-SH2结构域通过~120°旋转,从而使N-SH2结构域移位远离活性位点。shp099样变构抑制剂不能有效地结合这种活性构象,如C)所述
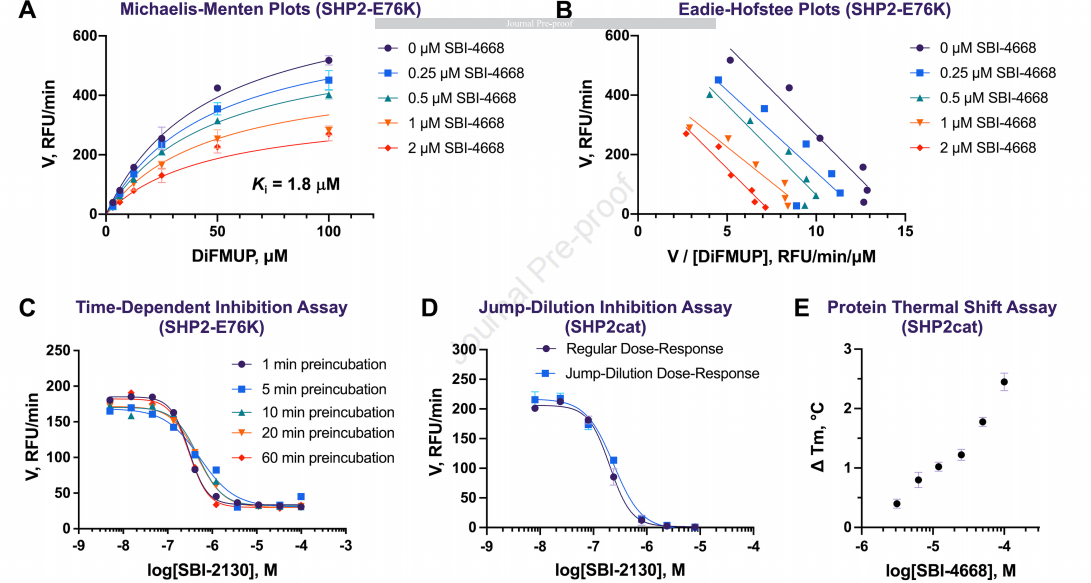
图2:SHP2抑制剂的作用机制、抑制作用及结合作用的研究
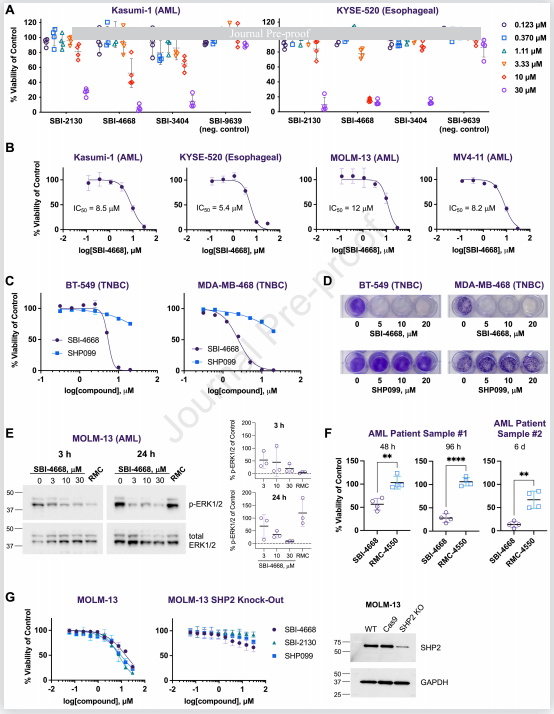
图3:SHP2抑制剂在细胞癌模型和患者来源的AML样本中的疗效和选择性
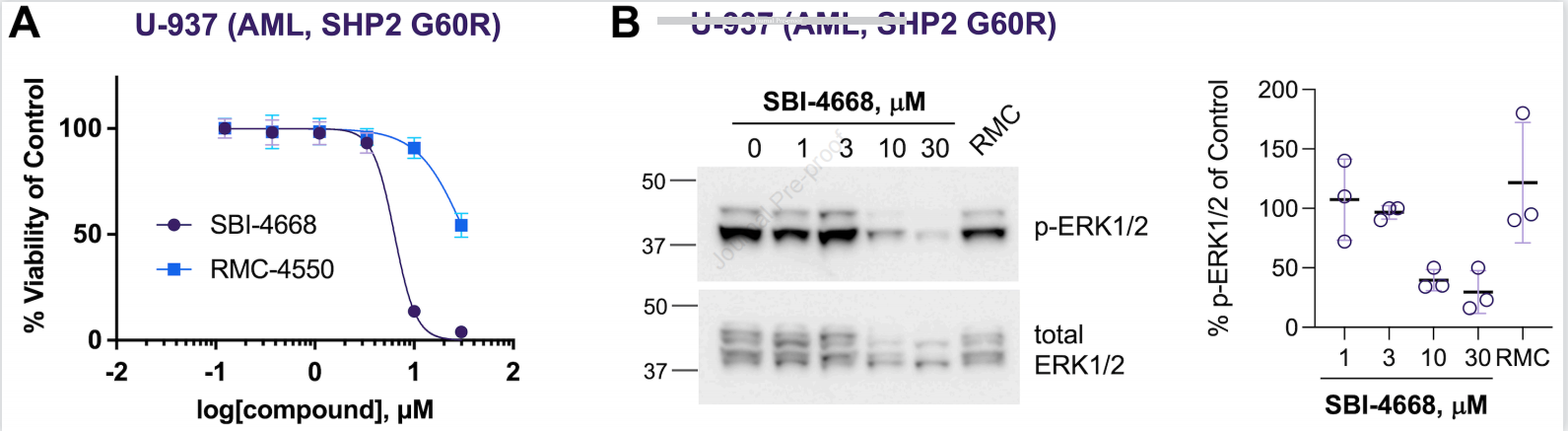
图4:SBI-4668在表达SHP2致癌变异G60R的U-937AML细胞中的SBI-4668的评价。A)U-937AML细胞在不同浓度的SBI-4668或SHP2变构抑制剂RMC-4550存在下培养3d后的细胞活力。细胞活力以DMSO载体对照的百分比表示,代表平均±SD(n=4),并使用非线性回归(对数[抑制剂]vs.归一化响应,变量斜率)拟合曲线。B)SBI-4668或SHPKRK1/2(RRK-R4小时的ERK1/2)总细胞裂解物的免疫印迹分析。p-ERK1/2水平的定量显示为DMSO(车辆)对照的百分比,并代表了来自三个独立实验的数据(平均±SD)
变构抑制SHP2的化合物正在I/II期临床试验中,无论是作为单一治疗,还是与其他RTK/Ras通路和免疫检查点抑制剂联合使用。新的SHP2变构抑制剂可能最终被证明对许多癌症的治疗具有变革作用。然而,由于其独特的作用机制,它们可能对由SHP2致癌突变形式驱动的癌症患者无效,最显著的是儿童和急性白血病。在所有血癌中,SHP2功能获得突变率最高的儿童发生在青少年骨髓单核细胞白血病(JMML)中,在这些儿童中,高达42%的白血病发生是由SHP2变异驱动的。
通过生化和生物物理评估,可以精确定位呋喃苯甲酰胺抑制剂与SHP2的磷酸酶结构域的相互作用。根据时间依赖性抑制、跳跃稀释抑制和质谱分析,可以排除通过添加到该系列化合物共同的烯酮双键上而产生的一种可能的共价机制。有趣的是,米凯利斯-Menten动力学实验表明,化合物并不直接与底物结合竞争。这一观点进一步得到了SAR研究的支持,其中底物相似性增加的类似物的效价降低,这表明SBI-2130、SBI-4668和相关类似物可能不与催化口袋中的磷酸盐结合环结合。
研究者表明,未来的研究将以确定化合物与SHP2的确切结合位点是必要的。这类研究还将使基于结构的、合理的设计额外的类似物,并进一步提高其效力和选择性。
原始出处:
Raveendra-Panickar D, Finlay D, Layng FI, Lambert LJ, Celeridad M, Zhao M, Barbosa K, De Backer LJS, Kwong E, Gosalia P, Rodiles S, Holleran J, Ardecky R, Grotegut S, Olson S, Hutchinson JH, Pasquale EB, Vuori K, Deshpande AJ, Cosford NDP, Tautz L. Discovery of novel furanylbenzamide inhibitors that target oncogenic tyrosine phosphatase SHP2 in leukemia cells. J Biol Chem. 2021 Dec 9:101477. doi: 10.1016/j.jbc.2021.101477. Epub ahead of print. PMID: 34896393.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#抑制剂#
46
#JBC#
39
#致癌#
43
#SHP2#
35
#磷酸酶#
37
未来可期
71
学习了
80