JAD:Meta分析揭示老年痴呆铁代谢异常新规律
2014-06-14 西湖营养 西湖营养
近日,国际权威学术期刊Journal of Alzheimer’s Disease(老年痴呆症杂志)发表了浙江大学公共卫生学院王福俤研究组题为“Perturbed Iron distribution in Alzheimer’s disease serum, cerebrospinal fluid and selected brain regions: a systematic rev

近日,国际权威学术期刊Journal of Alzheimer’s Disease(老年痴呆症杂志)发表了浙江大学公共卫生学院王福俤研究组题为“Perturbed Iron distribution in Alzheimer’s disease serum, cerebrospinal fluid and selected brain regions: a systematic review and meta-analysis”的最新研究成果[1]。
该Meta分析成果在充分肯定铁代谢异常与老年痴呆的密切关联性的同时,从根本上颠覆了“铁过载是老年痴呆患者的典型特征”的传统观点,并通过充分数据证实老年痴呆患者血清铁显著低于正常对照人群,且往往伴有(轻度)缺铁性贫血,而特定脑区存在高铁蓄积。该研究成果提示,机体铁稳态失衡在老年痴呆发生发展中发挥关键作用,阻止或降低脑组织高铁蓄积是老年痴呆防治的重要措施。
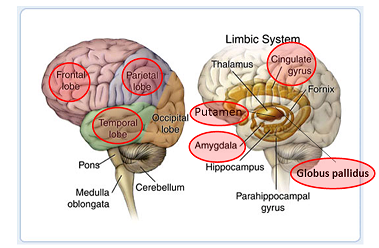

老年痴呆高铁脑区分布模式图(红圈为老年痴呆患者高铁脑区)
必需微量元素铁是体内合成血红蛋白、肌红蛋白的重要原料,也是一系列氧化还原反应系统中许多酶的辅酶,参与氧的运输、细胞呼吸等重要生理过程。因此,铁稳态代谢调控在维持机体新陈代谢中具有重要作用。铁缺乏可导致细胞生长停滞甚至死亡,人体表现贫血症状;但铁过量却同样对细胞有害,过量铁会产生自由基进一步对细胞成份如DNA、蛋白质及脂质体造成损伤,影响细胞功能。正是由于高铁的细胞毒作用,早在上世纪90年代高铁蓄积是否促发老年痴呆的问题就已经引起科学界的高度重视。
老年痴呆,又通常被称为阿尔茨海默病,是一种以进行性认知功能障碍为特征的神经退行性疾病,其典型的神经病理改变是患者脑内β-淀粉样蛋白(β-amyloid,Aβ)沉积和神经元细胞内的纤维缠结(neuro fibrillary tangles,NFTs)。有研究发现铁会选择性地在Aβ沉积的脑区蓄积;另有研究表明在出现纤维缠结的神经元细胞中存在铁过量现象。近年来,最新发表的研究也为铁与老年痴呆关联提供了重要证据,即Aβ淀粉样沉淀的前体蛋白APP的mRNA具有铁的响应元件,它的翻译过程是受铁含量调控,并且APP蛋白还具有铁的氧化活性可以将2价铁氧化成3价,从而促进铁从神经元细胞中排出(Duce JA, et al. Cell.2010);多项研究还发现铁代谢基因突变与老年痴呆症的发病风险呈正相关(Wang Y, et al. Can J Neurol Sci. 2013)。这些研究都提示铁代谢在老年痴呆症发生发展中扮演着某种角色。

为进一步明确铁稳态代谢在老年痴呆症发生中作用,王福俤研究组开展了基于此的荟萃分析研究。在王福俤教授的指导下,博士研究生陶云龙通过数据库检索共确定了2556篇相关研究报道;再通过论文题目与摘要筛选,确定105篇论文继续分析;最终将43篇研究文献纳入综合深度分析。该研究通过对老年痴呆患者血清、脑脊液及12个脑区铁含量水平的系统性荟萃分析(Meta-analysis),发现老年痴呆症患者血清铁含量显著低于正常对照人群,脑脊液中铁含量没有明显差异。更有意义的发现是,老年痴呆患者脑组织存在高铁蓄积现象,高铁蓄积并不是遍布全脑区域,12个脑区中铁含量呈现出不同的变化趋势,铁选择性地在额叶、顶叶、颞叶、杏仁核、尾壳核、苍白球及尾状核7个特定的脑区高度蓄积(如图)。
该研究从全新的角度揭示了老年痴呆患者铁代谢异常新规律,虽然这种特异脑区高铁蓄积的机制尚不清楚,但已充分证实老年痴呆的治疗不能简单地采用低铁饮食或全身的祛铁治疗,阻止特定脑区高铁蓄积以及特定脑区的祛铁治疗才是老年痴呆防治的根本举措。
该研究得到了国家科技部、国家自然科学基金委、浙江大学和中国科学院的经费资助。
原始出处:
Tao Y, Wang Y, Rogers JT, Wang F.Perturbed Iron Distribution in Alzheimer's Disease Serum, Cerebrospinal Fluid, and Selected Brain Regions: A Systematic Review and Meta-Analysis. J Alzheimers Dis. 2014 Jun 10.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#MET#
27
#Meta#
37
#铁代谢#
33
#新规#
35
#代谢异常#
44