阿斯利康的TSLP单抗tezepelumab治疗严重哮喘,III期临床成功
2020-11-10 MedSci原创 MedSci原创
“tezepelumab不同其他哮喘生物药物,是通过阻断胸腺基质淋巴细胞生成素(TSLP)发挥作用。”
阿斯利康和安进公司宣布其tezepelumab用于严重、无法控制的哮喘患者的III期研究达到了主要终点。在NAVIGATOR试验中,与安慰剂加标准治疗相比,将tezepelumab单克隆抗体添加至标准治疗后,在52周内显示出年平均哮喘急性发作率(AAER)的显着降低和临床改善。
在基线嗜酸性粒细胞计数低于300细胞/mcL的患者亚组中,该研究也实现了其主要目标,即AAER的显着降低和临床改善。在基线嗜酸粒细胞计数低于150细胞/mcL的亚组患者中,AAER也有类似的下降。
阿斯利康生物药物研发执行副总裁Mene Pangalos指出:“tezepelumab不同于其他哮喘生物药物,是通过阻断胸腺基质淋巴细胞生成素(TSLP)发挥作用。”
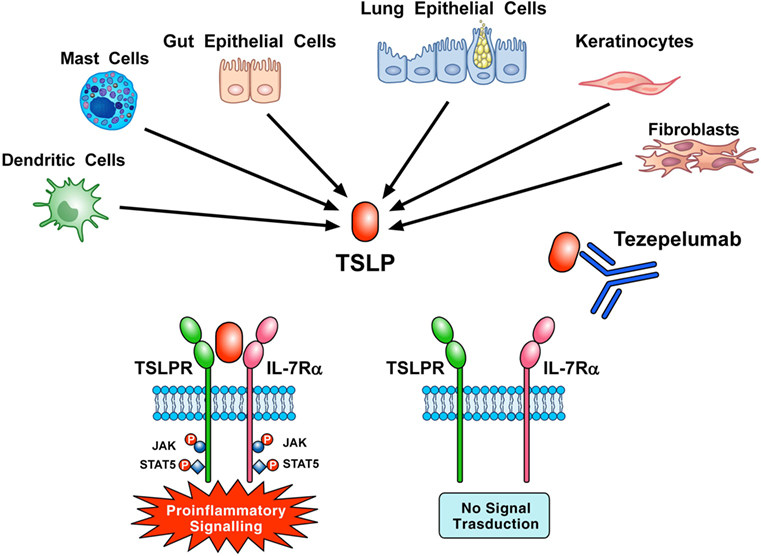
图片来源:https://www.frontiersin.org/articles/10.3389/fimmu.2018.01595/full
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#mAb#
29
#PE#
29
#III#
32
#I期临床#
36
#严重哮喘#
34
#II期临床#
32
#III期#
30
#Tezepelumab#
0
#PEL#
23
学习了、涨知识了!
0