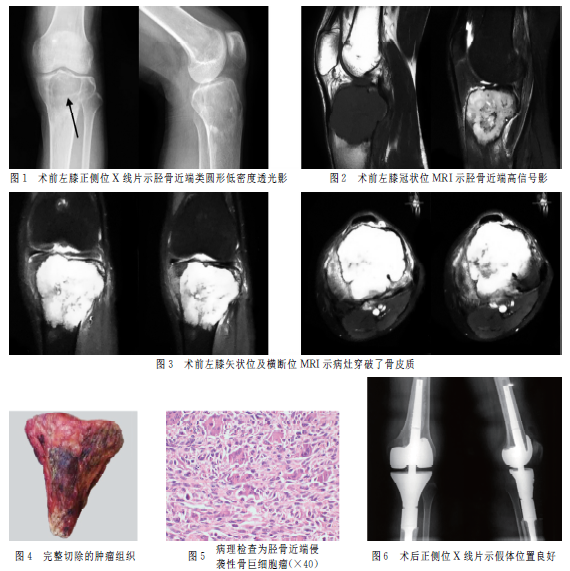
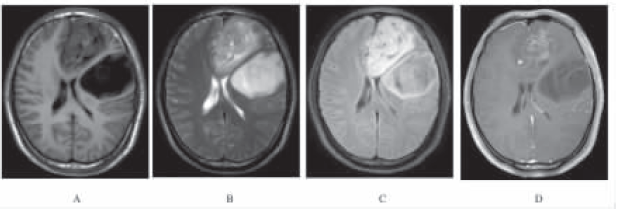
多中心骨巨细胞瘤伴肝肺转移1例
2019-11-25 刘凡 杨勇志 张德宝 实用骨科杂志
多中心骨巨细胞瘤(MCGCT)指同一患者发生的多于一处、并被组织病理学证实的骨巨细胞瘤。骨巨细胞瘤多为单发病灶,作为其中一种类型,多中心骨巨细胞瘤极为罕见,其发病率不足骨巨细胞瘤患者的1%。目前关于多中心骨巨细胞瘤文献资料均以个案报道为主,缺少多中心大样本数据。笔者曾于2017年12月收治1例多中心骨巨细胞瘤合并肝肺转移患者,现将诊治过程报道如下。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#多中心#
24
#细胞瘤#
32
#骨巨细胞瘤#
55
#巨细胞#
35
#肺转移#
0
好
85