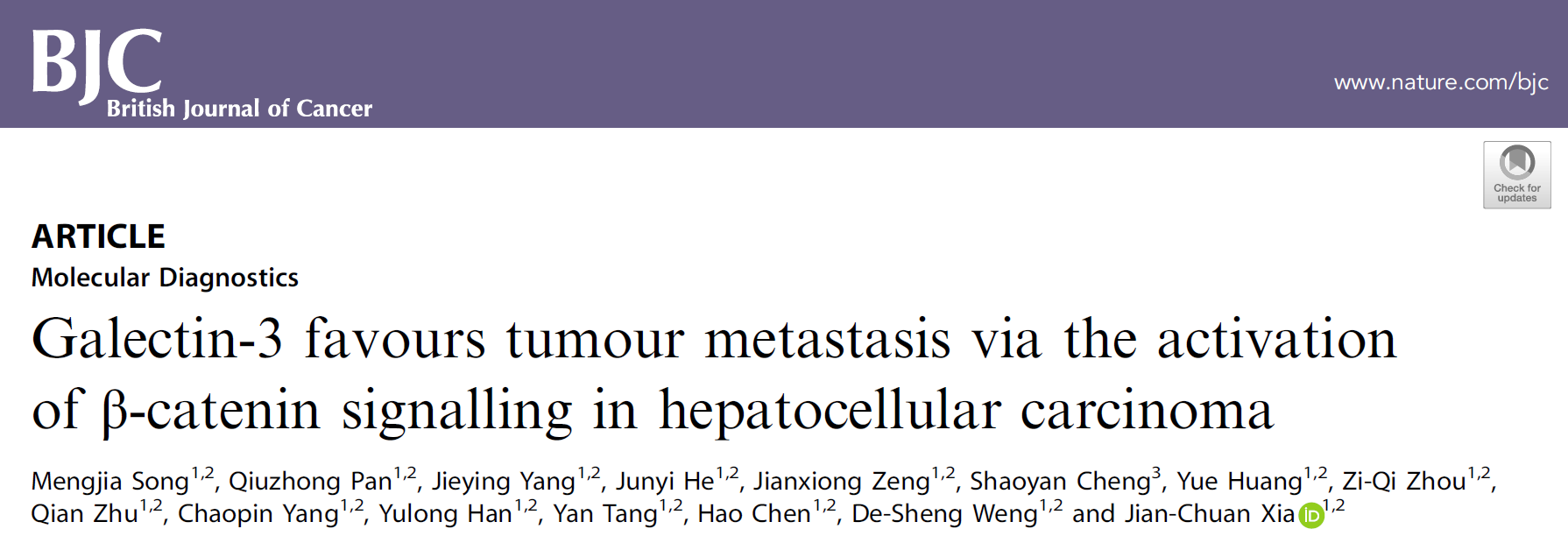
Br J Cancer:Galectin-3激活β-catenin信号通路促进肝癌转移
2020-08-30 QQY MedSci原创
肝细胞癌(HCC)作为最常见的癌症之一,是全球第二大癌症相关死亡原因,在中国约有50%的病例和死亡发生。尽管目前对于该疾病的治疗策略有所改善,但由于其高的转移性也限制了患者的长期存活率。
近年来的研究已确立了用于治疗HCC的抗血管生成疗法,其中索拉非尼(sorafenib)已被认为是不可切除或转移性HCC的二线治疗药物。然而,由于部分患者出现肿瘤转移且表现出索拉非尼耐药性,索拉非尼治疗策略只能使HCC患者的生存期平均延长3个月。因此,肝癌转移的分子机制研究显得尤为重要。
既往研究表明,Galectin-3(半乳糖凝集素3)与HCC患者的不良预后密切相关。Galectin-3是LGALS3基因编码的多功能蛋白,属于β-半乳糖苷结合蛋白家族。研究表明,Galectin-3能够以不同的方式在肿瘤发生发展过程中起着重要作用,包括血管生成、化疗耐药、免疫抑制和肿瘤转移等。而且既往研究已表明,Galectin-3是肝癌患者的预后因素,表明Galectin-3可能是肝癌发生发展甚至转移过程中的关键调节因子。
在该研究中,研究人员旨在探究Galectin-3对于HCC转移的贡献及其潜在分子机制。
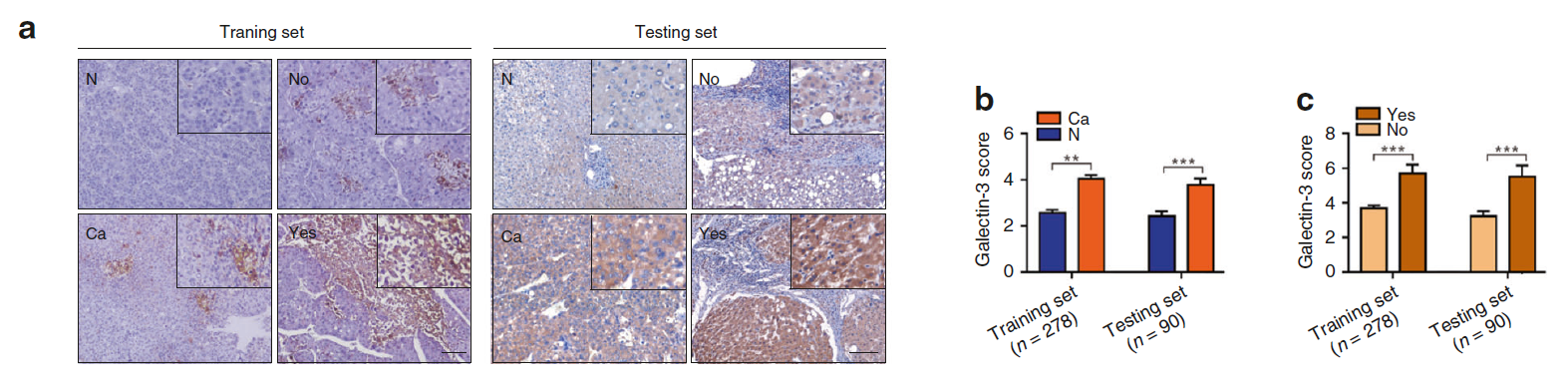
通过多组HCC患者的大规模研究分析发现,Galectin-3与血管的浸润和生存率低密切相关。Galectin-3能够参与HCC细胞中与肿瘤转移相关的各种过程,包括血管生成和上皮-间充质转化进程(EMT)。
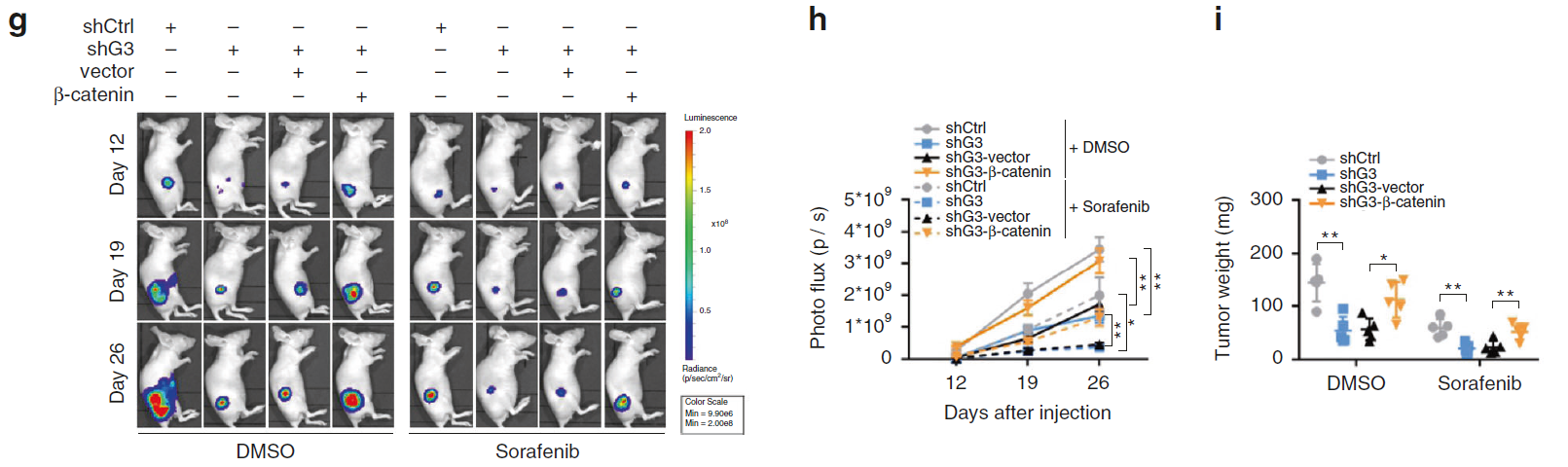
综上所述,该研究发现Galectin-3-β-catenin-IGFBP3/波形蛋白信号转导通路是影响HCC转移的主要机制,也为预测肿瘤的血管性转移和索拉非尼耐药性提供了潜在的生物标志物,并为HCC患者提供了潜在的治疗靶点。
原始出处:
Song, M., Pan, Q., Yang, J. et al. Galectin-3 favours tumour metastasis via the activation of β-catenin signalling in hepatocellular carcinoma. Br J Cancer (17 August 2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Galectin-3#
51
#信号通路#
33
#癌转移#
33
学习了
85
👍
83
学习了
86
学习了
83
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
43
学习
76
好
53