Front Oncol:吡咯替尼联合长春瑞滨治疗HER2阳性转移性乳腺癌的疗效:多中心回顾性研究
2021-10-22 MedSci原创 MedSci原创
研究表明,吡咯替尼加长春瑞滨治疗HER2+ MBC有效且毒性可控,特别是二线治疗患者,没有接受过拉帕替尼治疗的患者,以及有脑转移的患者。
吡咯替尼(Pyrotinib)联合卡培他滨在中国被批准用于人表皮生长因子受体2 (HER2)阳性转移性乳腺癌(MBC)。同时,长春瑞滨是MBC的另一种重要的口服和静脉化疗方案。因此,吡咯替尼联合长春瑞滨(pyrotinib + vinorelbine)可能是一种新的治疗选择,特别是对于卡培他滨治疗失败的患者。来自国内学者开展了回顾性研究(clinicaltrials.gov (04517305)),评估真实世界中吡咯替尼+长春瑞滨治疗HER2+ MBC的疗效。相关结果发表在Frontiers in Oncology杂志上。
研究对象为2018年5月至2020年6月在中国6家机构接受吡格替尼 +长春瑞滨治疗的HER2+ MBC患者。评估治疗的无进展生存期(PFS)、客观缓解率(ORR)、总生存期(OS)和毒性。
研究纳入97例患者,患者诊断时的中位年龄为53岁(范围26-74岁)。16例患者为新发IV期乳腺癌(16.5%)。此外,41.2%的患者有三个以上的转移部位,最常见的三个转移部位是肺(45.4%)、骨(40.2%)和肝(35.1%)。另外67.0%的患者有内脏转移,23例(23.7%)有脑转移。几乎所有患者都接受过抗HER2治疗,其中97.9%的患者接受曲妥珠单抗治疗,50.5%的患者接受拉帕替尼治疗。此外,67%的患者在吡咯替尼联合长春瑞滨之前接受了2线或更多的系统治疗。
共有92.8%的患者以标准的400 mg/d剂量开始接受吡格替尼治疗,而7.2%的患者以320 mg/d剂量开始接受吡格替尼治疗。此外,16(16.5%)和12(12.4%)例患者分别经历了吡格替尼的剂量减少和治疗中断。74.2%的患者口服长春瑞滨,25.8%的患者静脉注射长春瑞滨。13例(13.4%)患者因不良事件导致长春瑞滨剂量减少,6例(6.2%)患者中断长春瑞滨治疗。没有患者因不良反应而永久停止治疗。
所有患者均纳入PFS分析。在中位随访8.7个月时,52例患者病情进展,mPFS为7.8个月(4.7-10.8)。
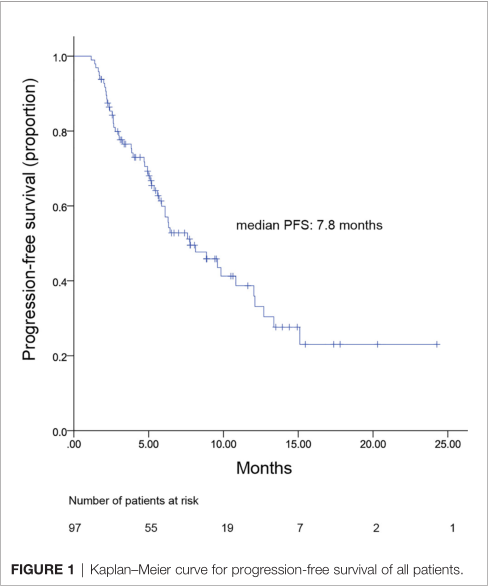
PFS
二线使用吡咯替尼加长春瑞滨治疗患者的mPFS为12.0个月(范围3.8-20.2),三线或以上治疗的mPFS为6.4个月(4.0-8.9)。只有2例患者接受一线治疗,尚不足以计算mPFS。三线或以上治疗组的mPFS短于二线治疗组;然而,差异不显著(p = 0.225 2)。

二线或后线PFS比较
此外,在接受吡格替尼+口服长春瑞滨或静脉注射长春瑞滨的患者之间的mPFS无显著差异(7.8 vs. 6.4个月,p = 0.871)。
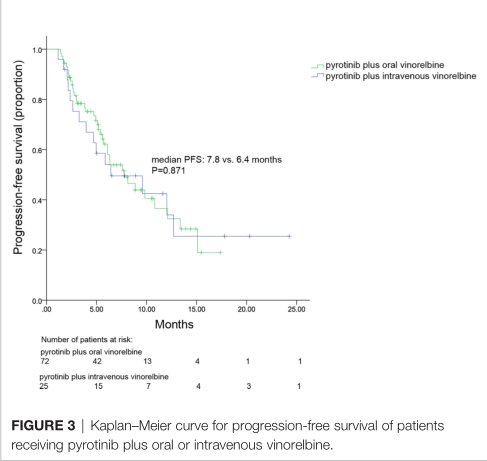
长春瑞滨口服或静脉PFS比较
脑转移患者的总mPFS(考虑颅内和颅外病变)为6.3个月(范围,3.4-9.2)。此外,有脑转移和无脑转移患者的PFS无差异(6.3 vs. 8.1个月,p = 0.825)。OS数据还不成熟。
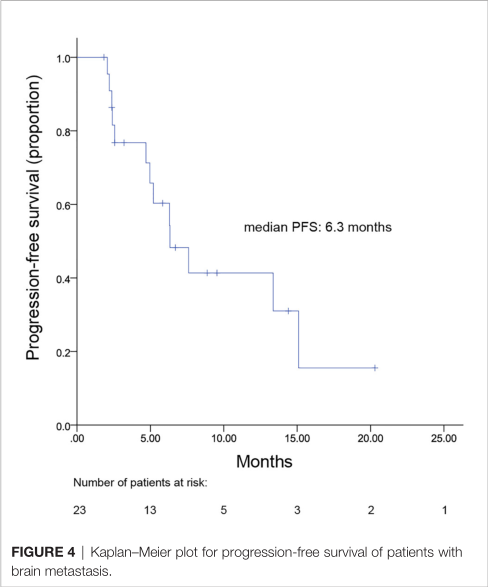
脑转移PFS
共有96例患者纳入ORR分析。无患者达到CR, 33例为PR, ORR为34.3%。
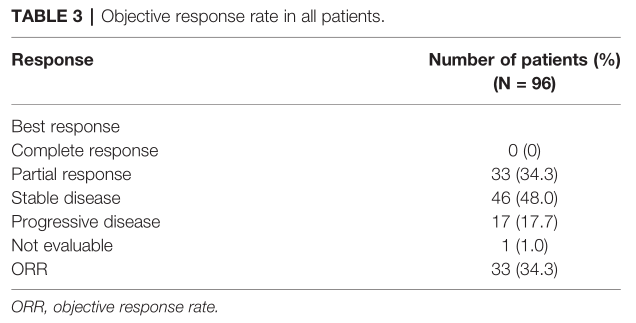
ORR
单因素分析表明,年龄(<50岁 vs ≥50岁)、激素受体状态(阳性vs阴性)、DFI (>1年vs. ≤1年),转移部位数量(≤2 vs. >2)转移类型(内脏vs.非内脏),吡格替尼 +长春瑞滨治疗线数(2 vs. 3),或曲妥珠单抗耐药状态(耐药vs耐药)与mPFS在Log-rank分析中无显著相关性。既往使用拉帕替尼和未使用拉帕替尼的患者的mPFS分别为5.6个月和10.8个月。然而,在Cox多因素分析中,既往使用拉帕替尼并不是mPFS的独立预测因素。
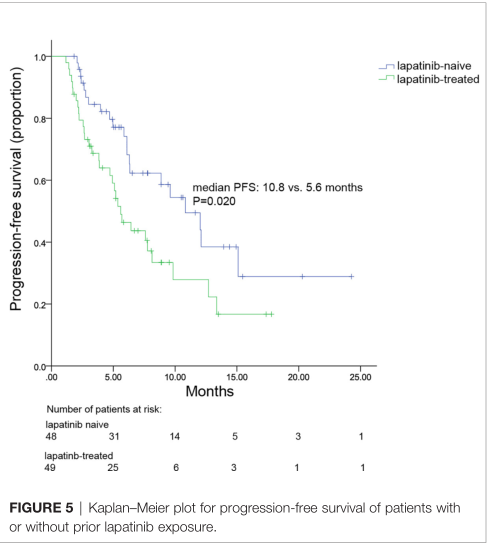
拉帕替尼使用与否PFS比较
研究报告3-4级AEs,最常见的是腹泻(22.7%),中性粒细胞减少(7.2%),白细胞减少(4.1%;无治疗相关死亡报告。总的来说,吡格替尼联合长春瑞滨的安全性是可控和可耐受的。
综上,研究表明,吡咯替尼加长春瑞滨治疗HER2+ MBC有效且毒性可控,特别是二线治疗患者,没有接受过拉帕替尼治疗的患者,以及有脑转移的患者。
原始出处:
Li Y, Qiu Y, Li H, Luo T, Li W, Wang H, Shao B, Wang B, Ge R. Pyrotinib Combined With Vinorelbine in HER2-Positive Metastatic Breast Cancer: A Multicenter Retrospective Study. Front Oncol. 2021 Apr 20;11:664429. doi: 10.3389/fonc.2021.664429. PMID: 33996589; PMCID: PMC8120312.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Oncol#
22
#HER2阳性转移性乳腺癌#
27
#多中心#
23
#HER2阳性#
43
#转移性#
22
#回顾性研究#
23