Front Oncol: 以吡格替尼(Pyrotinib)为基础治疗HER2+晚期乳腺癌患者的疗效:多中心回顾性研究
2021-10-22 yd2015 MedSci原创
研究表明,以吡格替尼为基础的治疗在HER2+患者中显示出良好的疗效且耐受性良好,尤其是≤2线治疗以及联合卡培他滨方案。
乳腺癌是世界上最常见的恶性肿瘤之一。随着早期发现和有效治疗的发展,乳腺癌的死亡率已经下降。然而,乳腺癌仍然是一个重要的死亡原因(2,3)。人表皮生长因子受体2 (HER2)阳性是一个关键的致癌驱动基因,其发病机制主要是PI3K/Akt和MAPK通路的激活。HER2过表达发生在15%- 20%的乳腺癌中。HER2阳性乳腺癌具有侵袭性,预后较差。抗HER2药物,如曲妥珠单抗、帕妥珠单抗、拉帕替尼和T-DM1,已经显著提高了her2阳性乳腺癌患者的生存。然而,耐药性仍然是一个主要挑战。因此,需要不断开发新的治疗方法。吡格替尼(Pyrotinib)是一种新开发的不可逆的泛-ErbB受体酪氨酸激酶抑制剂,抑制HER1、HER2和HER4。在一项开放标签II期研究中,与拉帕替尼+卡培他滨相比,吡格替尼+卡培他滨在her2阳性乳腺癌患者中的无进展生存期(PFS)明显更长(18.1个月vs 7.0个月,p<0.001),客观缓解率(ORR)更高(78.5% vs 57.1%, p<0.05)。此外,一项随机III期试验(PHOEBE)纳入了267名此前接受过曲妥珠单抗治疗的患者。结果显示,接受吡格替尼+卡培他滨治疗的患者的中位PFS (mPFS)明显长于接受拉帕替尼+卡培他滨治疗的患者(12.5个月vs 6.8个月,P <0.0001)。吡格替尼+卡培他滨治疗组的ORR高于拉帕替尼+卡培他滨治疗组(67.2% vs 51.5%)。然而,在临床实践中,吡咯替尼对不同基线特征患者的疗效鲜有报道。因此,来自江苏团队开展一项真实世界研究,评估吡格替尼再HER2阳性晚期乳腺癌患者的疗效。相关结果发表在Frontiers in Oncology杂志上。
从2019年2月至2020年4月,共纳入141名HER2阳性乳腺癌患者。最后一次随访时间是2021年2月。所有患者接受以吡格替尼为基础的治疗,每21天为一个周期。主要终点为无进展生存期(PFS)。
141例患者中,中位年龄为52岁(范围29-78岁)。136例(96.5%)患者ECOG <2;激素受体阳性占56.0%。转移灶分布在脑(14.9%)、肝(31.2%)、骨(44.0%)和肺(54.6%)。
104例(73.8%)患者接受了以吡格替尼为基础的治疗作为二线或后线治疗。100例(70.9%)患者开始使用400mg的吡格替尼治疗,39例(27.7%)患者开始使用320mg, 2例(1.4%)患者开始使用160mg。这些患者还接受了卡培他滨(55.3%)、曲妥珠单抗(17.7%)和内分泌治疗、放疗或抗血管生成药物(3.5%)的治疗方案。只有11例(7.8%)患者接受了吡格替尼单药治疗。
截止到2021年2月,中位随访时间为11.3个月(范围为1.0-26.4个月),52例(45.6%)患者随访超过1年。58例(41.1%)患者仍在接受吡格替尼治疗。吡格替尼为基础治疗患者的中位PFS (mPFS)为12.0个月(95%CI, 8.1-17.8)。

总体PFS
在有肝转移的患者中,mPFS为8.7个月(95%CI, 6.3-15.4),而无肝转移的患者为12.3个月(95%CI, 8.8-23.3) (HR=0.72;95%CI,0.44-1.18;P=0.174)。
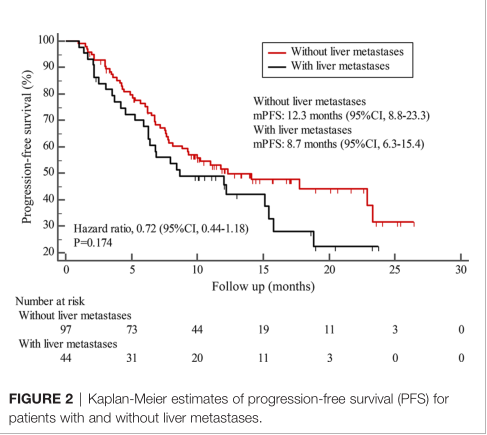
有无肝转移PFS
接受吡格替尼治疗>2线患者的PFS短于≤2线治疗患者,分别为8.4个月 (95%CI, 5.9-15.4) 和15.1个月(95%CI, 9.3-22.9)(HR=0.69; 95%CI, 0.44-1.10; P=0.109)。
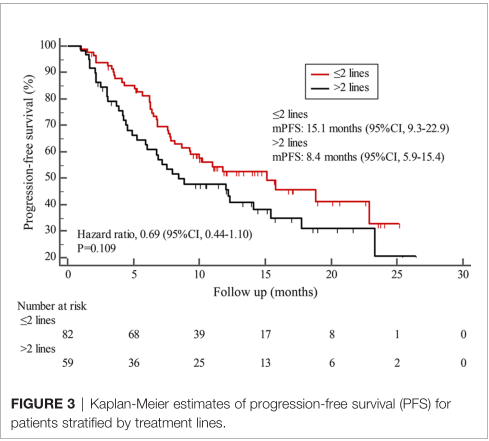
不同治疗线数PFS
先前接受过曲妥珠单抗的患者mPFS为12.2个月(95%CI, 7.9- 18.8),而未接受过曲妥珠单抗的患者mPFS为11.8个月(95%CI, 6.8-22.9) (HR=1.12;95%CI,0.56-2.25;P=0.732)。

既往接受过或无的PFS
此外,联合卡培他滨治疗方案与非联合卡培他滨治疗方案患者的mPFS分别为15.1个月(95%CI, 10.0-18.8)和8.4个月(95%CI,6.7-22.9) (HR=1.51;P=0.072)。

联合卡培他滨或无PFS
此外,在脑转移患者中,估计6个月的PFS率为70.0%,12个月的PFS率为60.0%。截至数据截止日期,中位OS尚未达到。
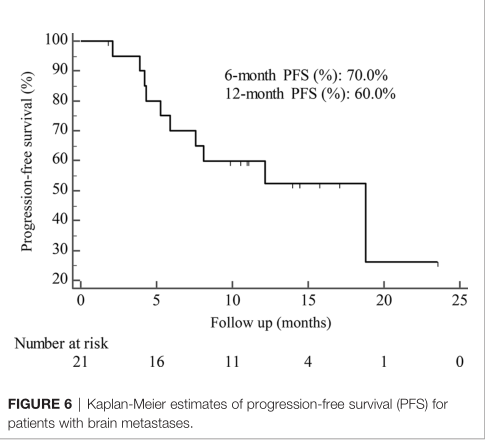
脑转移患者PFS
对70例可测量病变的患者进行反应评估。ORR为38.6%,DCR为85.7%。1例(1.4%)患者完全缓解,26例(37.1%)患者部分缓解。33例(47.1%)患者病情稳定,10例(14.3%)患者病情进展。
14例患者没有可用的安全性数据,其余127例患者纳入安全性评估。所有级别和3级不良事件(AEs)分别有123例(96.9%)和14例(11.0%)报告。最常见的AE为腹泻(85.0%),但只有6例(4.7%)报告3级腹泻。此外,AEs≥15%患者发生的包括贫血(37.0%)、白细胞减少(24.4%)、呕吐(24.4%)、中性粒细胞减少(22.0%)和高胆红素血症(17.3%)。没有治疗相关死亡的报告。

不良反应
综上,研究表明,以吡格替尼为基础的治疗在HER2+患者中显示出良好的疗效且耐受性良好,尤其是≤2线治疗以及联合卡培他滨方案。
原始出处:
Zhang L, Wu X, Zhou J, Zhu M, Yu H, Zhang Y, Zhao Y, Han Z, Guo Y, Guan X, Wang X, Xu H, Sun L, Zhang J, Zhuang M, Xie L, Yu S, Chen P, Feng J. Pyrotinib in the Treatment of Women With HER2-Positive Advanced Breast Cancer: A Multicenter, Prospective, Real-World Study. Front Oncol. 2021 Jul 16;11:699323. doi: 10.3389/fonc.2021.699323. PMID: 34336688; PMCID: PMC8322968.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Pyrotinib#
30
#Oncol#
32
#多中心#
24
#乳腺癌患者#
24
#回顾性研究#
20
已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读
40