夜班熬的是命!上海交大研究发现,熬夜、上夜班,与主要心血管不良事件风险增加92%有关
2022-08-07 医诺维 医诺维
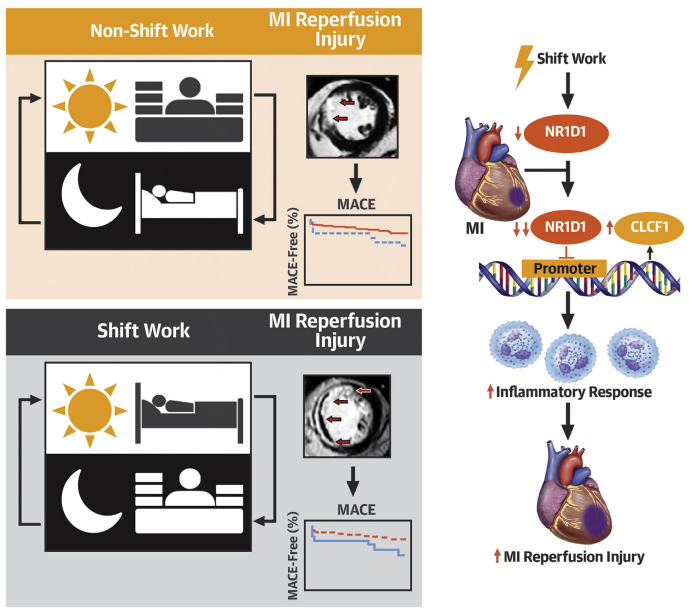
该研究表明,熬夜、上夜班导致生物节律紊乱,进一步诱发NR1D1表达降低,导致主要心血管不良事件风险增加。强调了维持节律稳态是一个潜在的心肌保护策略,为改善心肌梗死患者预后提供了新思路。
睡眠是人体的一种修复过程,可以恢复精神和解除疲劳。人的一生中,大约三分之一的时间是在睡眠中度过,良好的睡眠是国际社会公认的三项健康标准之一,而睡眠时间过短或睡眠不佳均会影响健康。
俗话说,“熬夜一时爽,一直熬夜火葬场”。在当今社会,熬夜已成为许多年轻人的新常态。经常熬夜会给身体带来非常大的危害,例如熬夜会引起免疫功能失调、生物钟紊乱等,更严重的是,长期熬夜还会引发猝死。
生物钟,已得到科学家的广泛研究。昼夜节律赋予了人类行为和生理学的时间模式,使身体内在与外在环境的预期变化保持一致,被扰乱的昼夜节律会对健康产生影响。
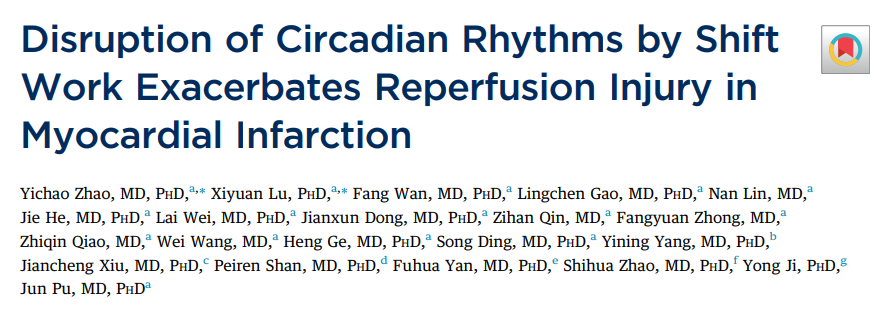
近日,上海交通大学附属仁济医院卜军团队在《美国心脏病学会》期刊上发表了一篇题为" Disruption of Circadian Rhythms by Shift Work Exacerbates Reperfusion Injury in Myocardial Infarction "的研究论文。
该研究表明,熬夜或夜班工作等昼夜节律紊乱加重急性心肌梗死患者急诊再灌注术后心肌损伤,并导致长期临床预后不良。在5年的平均随访期间,与不上夜班的人相比,经常上夜班与主要心血管不良事件的风险增加92%有关。
急性心肌梗死,是指冠状血管突然堵塞,引起相应区域的心肌坏死。是影响我国国民生命健康的重大疾病,目前急性心血管事件具有昼夜节律特点已成共识,但是昼夜节律紊乱带来的心血管损伤风险却依然未明。
在这项前瞻性、多中心临床研究中,研究人员分析了412名心肌梗死患者的数据,年龄在52-62岁之间,90%以上是男性,其中102名属于轮班工作者。与不上夜班的患者相比,经常上夜班的人通常更年轻、BMI更高。
所有患者均在心梗发生后的12小时内接受了急诊再灌注手术,并于术后1周内进行了心脏磁共振评估心肌梗死面积,以及主要不良心血管事件,包括死亡、心肌梗死、心力衰竭和脑卒中等。
研究发现,与不上夜班的患者相比,经常上夜班显著增心肌梗死面积,心脏微血管阻塞发生率明显更高。
在平均5年随访期间,共发生了75例心血管不良事件。其中,死亡6例,心肌再梗死14例,心力衰竭48例,中风7例。
调整混杂因素后分析发现,与不上夜班的患者相比,经常上夜班与发生主要心血管不良事件的风险增加了92%相关,心衰风险增加106%相关。

主要心血管不良事件的风险增加
在此基础上,研究人员利用动物模型对以上结果进行了验证。
在模拟上夜班的小鼠实验中,研究发现,与昼夜节律正常的小鼠相比,模拟上夜班的小鼠心肌梗死面积显著增加。此外,昼夜节律紊乱的小鼠心肌梗死术后死亡率也显著升高。
由于小鼠是夜行动物,研究人员又对绵羊进行了实验,研究得到了类似的结果。进一步验证了昼夜节律紊乱是导致术后心肌损伤加重和功能恶化的原因。
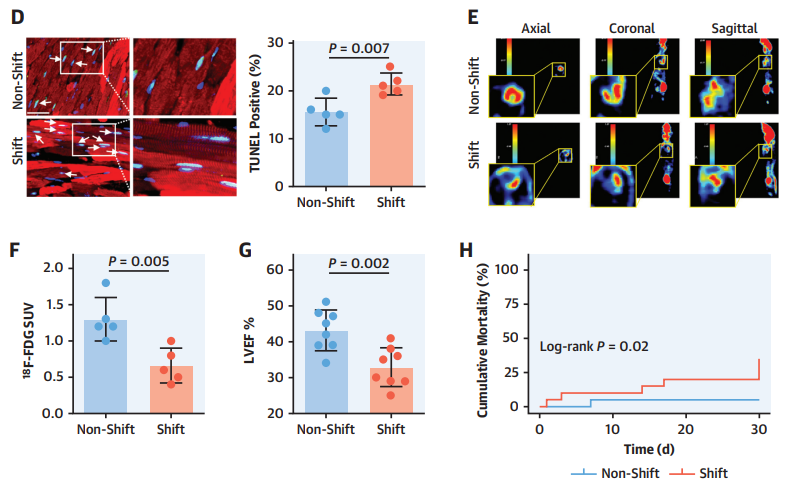
模拟夜班小鼠实验
在后续的进一步实验中,昼夜节律紊乱的小鼠心肌细胞核受体NR1D1表达显著降低。这意味着,NR1D1可能在昼夜节律失调诱导心肌损伤和功能障碍中发挥重要作用。
当研究人员敲除了小鼠NR1D1后发现,小鼠发生心肌梗死术后,心肌梗死面积明显更大,心肌活性和心功能也更差。
总之,该研究表明,熬夜、上夜班导致生物节律紊乱,进一步诱发NR1D1表达降低,导致主要心血管不良事件风险增加。强调了维持节律稳态是一个潜在的心肌保护策略,为改善心肌梗死患者预后提供了新思路。
论文链接:
https://doi.org/10.1016/j.jacc.2022.03.370
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#不良事件风险#
38
#研究发现#
46
#心血管不良事件#
42
#上海交大#
47
吓得只有辞职了😂
47