
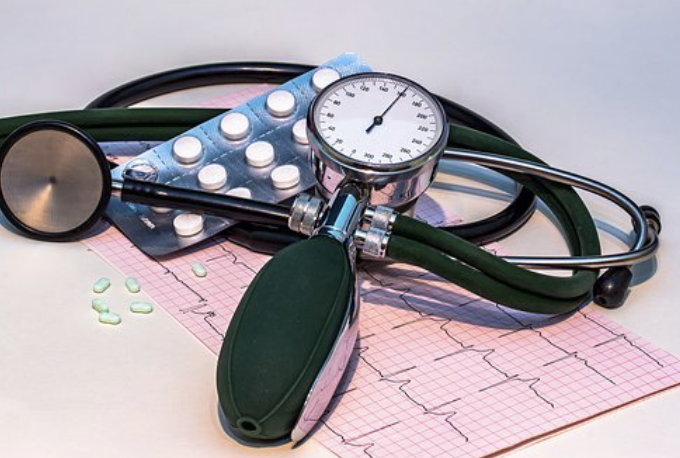
三个大型的试验:收缩压干预试验(SPRINT)、控制糖尿病心血管风险行动(ACCORD)血压试验和强化与标准流动降压以防止老年人功能衰退(INFINITY)试验。 这3个试验的结果均表明:随着血压控制的加强,白质病变(WML或leukoaraiosis)的进展较少,这是脑血管损伤的生物标志。
然而,强化治疗对认知障碍和痴呆的其他机制性标志物的影响还有待探讨。老年人痴呆的最常见原因是阿尔茨海默病(AD)。血管疾病是一种非常常见的合并症,可能是启动或加速AD神经病理学的一个因素。一些研究发现,治疗高血压可能会降低AD的发病率;
然而,目前还不清楚这可能是对AD相关神经变性或合并血管病理学的直接影响。AD的神经变性导致大脑萎缩,有利于但不限于特定的大脑区域,测量这些变化的生物标志物可能比下游认知或临床变量(如发生痴呆)对早期AD相关变化更敏感。
ACCORD和SPRINT都显示,与标准治疗相比,强化治疗的总脑容量(TBV)有小幅但有统计学意义的下降,尽管目前还不清楚这些差异在多大程度上反映了萎缩与水化状态等因素。
与AD相关的大脑变化有多种MRI生物标志物。研究最广泛的是海马萎缩,这是典型的轻度认知障碍和AD的标志。最近,对皮质变薄模式的评估和机器学习方法已经确定了类似AD萎缩的模式,这些模式通常比海马萎缩有更高的敏感性和特异性。其中一种方法被称为识别AD的空间模式(SPARE-AD),根据大脑与AD模式的整体相似性与正常的相似性,分配一个单一的全局分数。先前的研究还确定了与AD相关的白质完整性的变化,包括齿状束的各向异性(FA)下降和区域脑血流(CBF)的异常,如AD特征区域的灌注下降。
藉此,宾夕法利亚大学大的IlyaM. Nasrallah等人,提出假设:强化治疗与MRI的AD特异性大脑测量有关(即与海马体积、AD区域皮质厚度和SPARE-AD测量的较少萎缩有关;楔形束的FA减少较少;以及后扣带回的灌注增加)。
为了进行比较,他们还评估了几个假定的血管疾病的脑部MRI生物标志物的变化,特别是额部灰质体积、额部灰质灌注和胼胝体的FA。
该研究是收缩压干预试验(SPRINT MIND)的一项子研究,这是一项多中心的随机临床试验,比较了两种不同的降压策略的效果。50岁或以上的高血压、无糖尿病或中风病史的潜在参与者(n = 1267)被找来进行脑磁共振成像(MRI)研究。其中,205名参与者被认为不符合条件,269名不同意参与;673名和454名参与者分别在基线和4年随访时完成了脑磁共振成像;最终随访日期为2016年7月1日。分析从2019年9月开始,到2020年11月结束。
干预措施:参与者被随机分配到小于120毫米汞柱的收缩压目标(强化治疗:n = 356)或小于140毫米汞柱(标准治疗:n = 317)。
主要临床结局:海马体积的变化,AD区域萎缩的测量,后扣带脑血流,以及扣带束的平均各向异性。
在673名有基线MRI的招募患者中(平均[SD]年龄,67.3[8.2]岁;271名女性[40.3%]),454人在随机化后3.98(3.7-4.1)年的中位数(四分位数范围)完成随访MRI。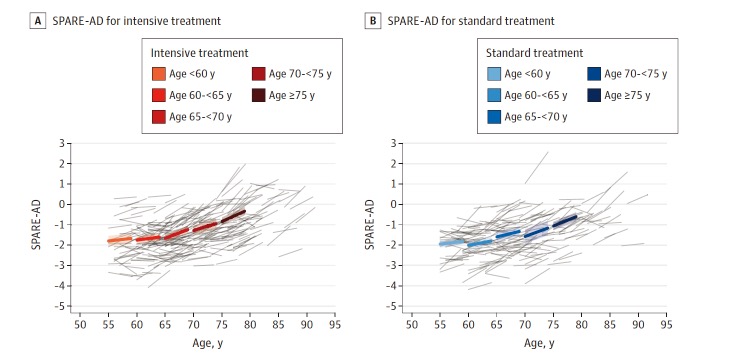
在强化治疗组,平均海马体积从7.45 cm3减少到7.39 cm3,而标准治疗组从7.48cm3减少到7.46cm3。
对AD区域萎缩、脑血流或平均各向异性的测量没有明显的治疗组差异。
这个研究的重要意义在于,发现了:与标准治疗相比,强化治疗与海马体积的小幅下降有关,但有统计学意义,这与强化治疗与总脑体积的更大下降有关的观察一致。然而,与标准治疗相比,强化治疗与AD的任何其他MRI生物标志物的变化无关。
原文出处
Nasrallah IM, Gaussoin SA, Pomponio R, Dolui S, Erus G, Wright CB, Launer LJ, Detre JA, Wolk DA, Davatzikos C, Williamson JD, Pajewski NM, Bryan RN; SPRINT Research Group. Association of Intensive vs Standard Blood Pressure Control With Magnetic Resonance Imaging Biomarkers of Alzheimer Disease: Secondary Analysis of the SPRINT MIND Randomized Trial. JAMA Neurol. 2021 May 1;78(5):568-577. doi: 10.1001/jamaneurol.2021.0178. PMID: 33683313; PMCID: PMC7941253.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Neurol#
31
。
61
理学物理标准治疗
63
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
42
认真学习
58