Radiology:结直肠癌肝转移病灶也有HCC相似的MRI表现
2021-05-04 shaosai MedSci原创
根治性肝切除术被认为是治疗结直肠癌肝转移(CRLM)的标准术式。迄今为止,切除CRLM的临床病理报告主要集中于恶性肿瘤的确诊和手术切缘的评估,但一些报告表明病理性血管浸的存在可影响患者的长期预后。
根治性肝切除术被认为是治疗结直肠癌肝转移(CRLM)的标准术式。迄今为止,切除CRLM的临床病理报告主要集中于恶性肿瘤的确诊和手术切缘的评估,但一些报告表明病理性血管浸的存在可影响患者的长期预后。血管侵犯门静脉、肝静脉或者胆管系统都可能是切除CRLM后患者预后不良的风险因素。
Gd-EOB-DTPA增强MRI对小于10mm的CRLMs的检测及表征优于CT,对术前准确的手术计划的制定至关重要。在HCC中,已有多项研究发现瘤周的早期不规则强化或较大的瘤周血流动力学改变提示微血管浸润。同时也有研究指出,Gd-EOB-DTPA增强MRI肝胆期所显示的瘤周低信号区提示微血管浸润。结合这些瘤周影像学表现可以更准确地预测肝细胞癌的微血管浸润和早期复发。然而据我们所知,尚无基于Gd-EOB-DTPA增强MRI预测CRLM微血管侵犯方面的相关报道。
近日,发表在Radiology杂志的一项研究探讨了CRLM周围Gd-EOB-DTPA增强MRI表现与病变病理血管浸润及患者远期预后的关系,为临床提供了一个术前准确评估血管浸润的无创影像学手段,为临床进一步制定最佳的手术方案并预测患者预后提供技术支持。
本项回顾性研究纳入了在2008年7月至2015年6月之间未接受新辅助化疗的行CRLM根治性手术的患者,所有患者均在术前接受了Gd-EOB-DTPA增强MRI检查。MRI的CRLM由三位腹部放射科医生评估。重新评估所有肿瘤标本中是否存在门静脉,肝静脉和胆管浸润。使用贝叶斯信息准则的Cox比例风险模型确定手术后无复发生存期(RFS)和总生存期(OS)的预测指标。选择先前报道的预后因素进行多变量分析。 中位随访期为60个月(范围9-127个月)。
本研究对106例患者(平均年龄65岁±12岁[标准差];68名男性)共148个CRLMs进行了评估。肿瘤周围胆管扩张与病理性门静脉浸润(敏感性:12/50 [24%];特异性:89/98 [91%];P = .02)、胆管侵犯(敏感性:8 / 19 [42%];特异性为116 / 129 (P = .001)、RFS较差(P = .03;风险比[HR] = 2.4[95%CI: 1.3, 4.2])及低OS 相关(P = 0.01;HR = 2.4[95%CI:1.2,4.9])。对于RFS和OS,通过多变量分析中的变量选择排除了CRLM周围早期增强和Gd-EOB-DTPA摄取减少,但这些结果与胆管扩张相结合可提供OS较差的预测因子(P = .001;HR = 3.3[95%可信区间:1.6,6.8])。
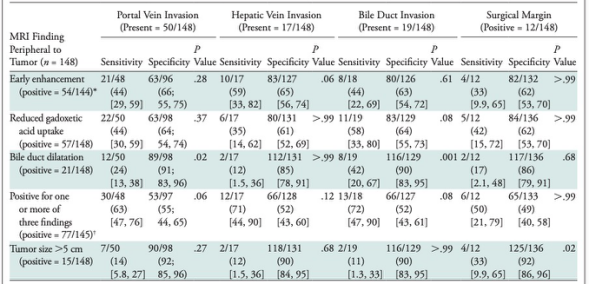
表 肿瘤周围MRI表现预测病理特征的敏感性和特异性。
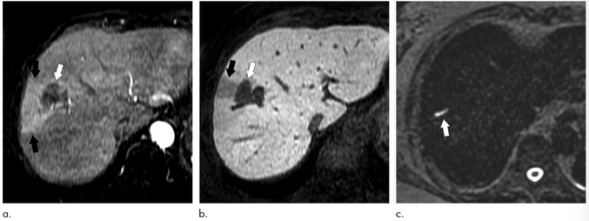
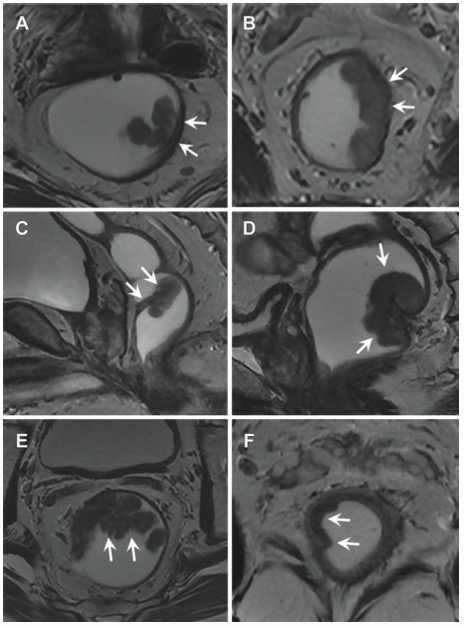
图 69岁女性,结直肠癌肝转移。(a)早期动脉期、(b)20分钟肝胆期、(c)重T2加权Gd-EOB-DTPA增强MRI图像。肿瘤呈环形强化(a白色箭头),肝胆期呈明显低信号(b白色箭头)。肿瘤周围呈楔形强化(a黑色箭头),肝胆期呈中低信号(b黑色箭头)。c线状高信号(箭头)提示胆管因肿瘤梗阻而扩张(箭头)。
综上所述,结直肠癌肝转移病灶周围MRI信号强度的改变及胆管扩张是预测未接受新辅助化疗的行根治性手术切除患者长期预后的重要因素,同时早期强化、钆酸摄取减少和肿瘤周围胆管扩张相结合也预示着该类患者远期预后较差。本研究结果显示,评估肿瘤周围影像学表现增加了术前常规MRI的临床价值,这为临床术前制定个性化治疗方案并预测患者预后提供了参考依据。
原文出处:
Yudai Nakai,Wataru Gonoi,Ryo Kurokawa,et al.MRI Findings of Liver Parenchyma Peripheral to Colorectal Liver Metastasis: A Potential Predictor of Long-term Prognosis.DOI:10.1148/radiol.2020202367
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









学习
65
#HCC#
55
#肝转移#
52
#结直肠#
45
#学习#h
86
值得学习!
63
好文章,谢谢分享。
61